Background: One of my favorite ED superstitions is that if someone says the word “quiet,” all hell is going to break loose. Many believe this superstition and as the ED inevitably gets busier as the day goes on, the person who said the Q word gets blamed for the volume; classic association being confused with causation. I have never heard the opposite…“oh it’s busy,” and when it slows down, no one ever gets upset for someone saying the B word. This is our own bias of work aversion in my humble opinion. In this day and age of evidence-based medicine, we finally have a tongue-in-cheek study that proves my point.
Background: One of my favorite ED superstitions is that if someone says the word “quiet,” all hell is going to break loose. Many believe this superstition and as the ED inevitably gets busier as the day goes on, the person who said the Q word gets blamed for the volume; classic association being confused with causation. I have never heard the opposite…“oh it’s busy,” and when it slows down, no one ever gets upset for someone saying the B word. This is our own bias of work aversion in my humble opinion. In this day and age of evidence-based medicine, we finally have a tongue-in-cheek study that proves my point.
From Research to Practice Ep6.0: The Q Word Superstition
[embedyt] https://www.youtube.com/watch?v=3xm_DnM5jho[/embedyt]
Also Be Sure to Checkout our YouTube Channel

What They Did:
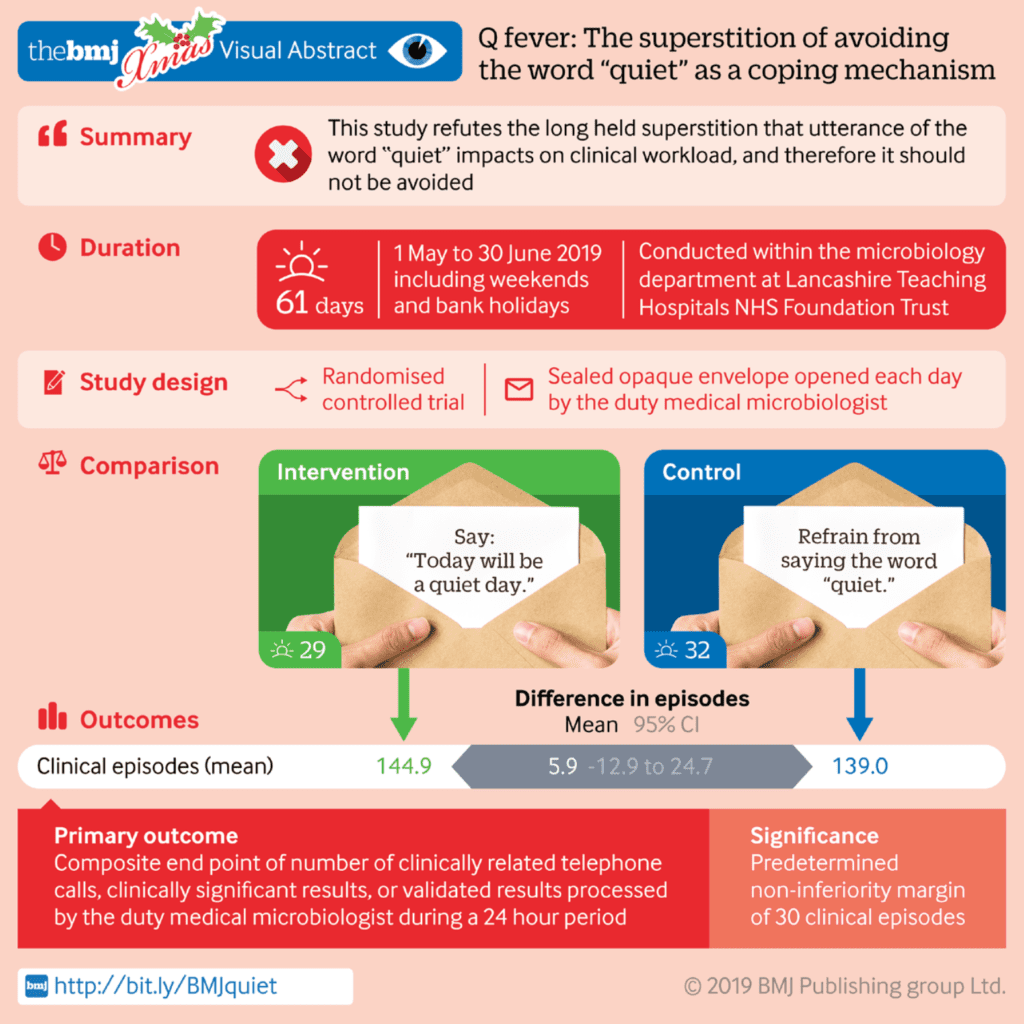
- Determining the validity of the superstition that saying the word “quiet” in a clinical setting increases workload.
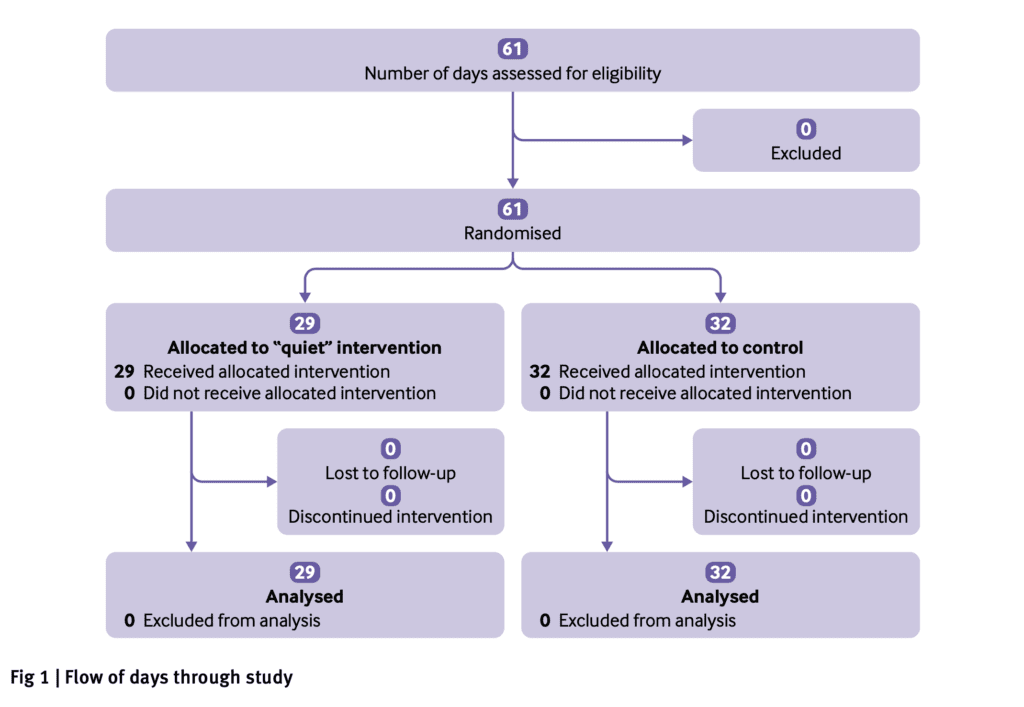
- Single center, prospective randomized controlled non-inferiority study
- Took place in the microbiology department of a teaching hospital in the UK
- 29 days randomly assigned in which staff were to say: “Today will be a quiet day” (intervention group) vs 32 days randomly assigned in which staff were to refrain from saying the word “quiet” (control group)
Outcomes:
- Primary: Mean overall workload: A composite of number of clinically related telephone calls, clinically significant results, or validated results processed by the on duty medical microbiology team during a 24 hour period referred to collectively as “clinical episodes” (A difference of 30 clinical episodes was considered the margin of non-inferiority)
- Secondary: Individual components of the primary outcome
Inclusion:
- Healthcare providers
Exclusion:
- N/A
Results:
-
Mean Clinical Episodes:
- Not Saying Quiet: 139.0
- Saying Quiet: 144.9
- Difference 5.9 (95% CI -12.9 to 24.7)
- No evidence of difference in workload was found between interventions with any of the four individual components of the primary outcome
-
Mean Clinical Episodes on Special Days:
- 3 Full Moon Days or Summer Solstice: 150.7
- Days Without a Full Moon or Summer Solstice: 141.4
- Mean Difference -9.3 (95% CI -53.7 to 35.1)
Strengths:
- Sample size calculations were based on data taken in the winter and the study took place at a traditionally quieter period (May to June)
- Analysis blinded to treatment allocation
- Clinical episodes were witnessed by other team members to ensure accuracy
- Minimized confounding by not disseminating the intervention to colleagues who worked in other departments
- Consecutive days were used, and all information was collected over the full 24hours of the day
- The margin of non-inferiority was prespecified before completion of the protocol and study start
- Analyses were repeated after adjustment for day of the week and bed occupancy as potentially important predictors of workload
- Also performed a post hoc analysis to evaluate whether workload increased on days with a full moon, solstices, or equinoxes, or a Friday the 13th day of the month
Limitations:
- Study took place in a single center, microbiology laboratory which may not extrapolate to an ED setting
- Could not control for the use of the word quiet within the other hospital departments
- Microbiology ward rounds were not included in the data collection
- Did not control for other confounding factors such as seasonal variation, number of microbiological samples received, or presence of black cats, or broken mirrors
- The pre-specified margin of inferiority was determined based on clinical judgment of the authors and colleagues and not from a formal consensus
- There was an imbalance in treatment allocation between weekdays and weekends
Discussion:
- The tone, enthusiasm, and audibility with which the “q word” was uttered was at the discretion of the duty member
- The study included 41 weekdays, two days with a full moon and one day of the summer solstice, and no Friday’s on the 13th day of the month
- Directly from the paper: “areas for further research include whether horse shoes placed outside patient isolation rooms can prevent the transmission of resistant organisms, whether a rabbit’s foot in theatre can reduce surgical site infections, a and whether being touched by a royal can cure tuberculosis.”
Author Conclusion: “The study findings refute the long-held superstition that utterance of the word “quiet” impacts on clinical workload, and therefore it should not be avoided. In the era of considerable staff shortages and increased work-related stress, doctors should look to other methods to increase resilience and protect their wellbeing and mental health.”
Clinical Take Home Point: Use of the “Q word” did not impact clinical workload in this single center study, should not be avoided, and maybe even encouraged, as the sentiment in wishing a colleague a quiet shift is a good one.
References:
- Brookfield CR et al. Q Fever – The Superstition of Avoiding the Word “Quiet” as a Coping Mechanism: Randomised Controlled Non-Inferiority Trial. BMJ 2019. PMID: 31852676
For More on This Topic Checkout:
- First10EM: Saying Quiet has no Effect in Medicine (Obviously)
- JournalFeed: Gosh, It’s Quiet – Does Saying the Q-Word Bring Disaster?
Post Peer Reviewed By: Anand Swaminathan, MD (Twitter: @EMSwami)
The post The Q Word Superstition appeared first on REBEL EM - Emergency Medicine Blog.