
 Background: Although Helmet CPAP is not something commonly used in the US, I think its nice to know what other potential options there are to help patients in the midst of a COVID-19 pandemic. Hypoxemic acute respiratory failure (hARF) is a well-known complication that can occur in patients with pneumonia. This has a high morbidity and mortality associated with it. An intermediary step prior to intubation is the use of noninvasive positive pressure ventilation (NIPPV) to stave off intubation. A more important question is does NIPPV in patients with pneumonia and hARF improve clinical outcomes? There have been no randomized clinical trials that have evaluated the clinical efficacy of helmet CPAP in patients with pneumonia suffering from hARF to date Helmet CPAP has also gained recent attention as an oxygenation tool for COVID19 pneumonia. The authors of this trial wanted to compare helmet CPAP vs oxygen therapy delivered by Venturi mask to reduce the proportion of patients requiring ETI in hARF due to pneumonia.
Background: Although Helmet CPAP is not something commonly used in the US, I think its nice to know what other potential options there are to help patients in the midst of a COVID-19 pandemic. Hypoxemic acute respiratory failure (hARF) is a well-known complication that can occur in patients with pneumonia. This has a high morbidity and mortality associated with it. An intermediary step prior to intubation is the use of noninvasive positive pressure ventilation (NIPPV) to stave off intubation. A more important question is does NIPPV in patients with pneumonia and hARF improve clinical outcomes? There have been no randomized clinical trials that have evaluated the clinical efficacy of helmet CPAP in patients with pneumonia suffering from hARF to date Helmet CPAP has also gained recent attention as an oxygenation tool for COVID19 pneumonia. The authors of this trial wanted to compare helmet CPAP vs oxygen therapy delivered by Venturi mask to reduce the proportion of patients requiring ETI in hARF due to pneumonia.
Paper: Brambilla AM et al. Helmet CPAP vs. Oxygen Therapy in Severe Hypoxemic Respiratory Failure Due to Pneumonia. Intensive Care Med 2014. PMID: 24817030
Clinical Question: Is Helmet CPAP superior to standard oxygen in the treatment of acute respiratory failure due to pneumonia?
What They Did:
- Multicenter, open-label, parallel-group, randomized controlled trial performed at 4 Italian centers
- Patients randomized to:
- Helmet CPAP (CPAP group)
- Flow of 90 – 140LPM, PEEP of 10cmH20, FiO2 set to maintain SpO2 of at least 92%
- Oxygen delivered through Venturi mask (Control group)
- FiO2 delivered set to maintain an SpO2 of at least 92%
- Both groups treated with antibiotics following the American Thoracic Society/Infectious Diseases Society of America (ATS/IDSA) guidelines
- Helmet CPAP (CPAP group)
Outcomes:
-
Primary: Percentage of patients meeting criteria for endotracheal intubation (ETI)
- Criteria Included:
- One or more major criteria (respiratory arrest, respiratory pauses with unconsciousness, severe hemodynamic instability (SBP <90mmHg), intolerance) OR
- At least two minor criteria (reduction of at least 30% of basal PaO2/FiO2 ratio, increase of 20% of PaCO2, worsening alertness, respiratory distress, SpO2 <90%, exhaustion)
-
Secondary:
- In-hospital mortality
- Hospital LOS
- Development of adverse events
- Improvement of gas exchange
- Criteria Included:
Inclusion:
- Age ≥18 years
- Severe hypoxemic acute respiratory failure (hARF) due to pneumonia (defined as PaO2/FiO2 ratio of at most 250 evaluated during oxygen therapy supplied for at least 15 min through a Venturi mask with an FiO2 of at least 0.50)
- RR of at least 30BPM
- Respiratory distress
Exclusion:
- Need for immediate intubation
- Acute respiratory acidosis (pH < 7.35 and/or PaCO2 >45mmHg)
- Unstable angina or acute MI
- SBP <90mmHg despite adequate volume resuscitation and/or use of vasopressors
- Severe arrhythmias
- Convulsions
- AMS
- Swallowing disturbance with increased risk of aspiration pneumonia
- Inability to protect the airway
- Recent facial trauma or burn
- Non-cooperative patient
- Presence of open wounds (head, thorax, abdomen
- Pregnancy
Results:
- 81 patients randomized
- Assessed 390 patients for eligibility
- 148 excluded due to acute CHF and/or COPD
- 161 excluded due to need for immediate intubation, acute respiratory acidosis, SBP <90mmHg with use of vasopressors, non-cooperative, acute MI, severe arrhythmias, etc…)
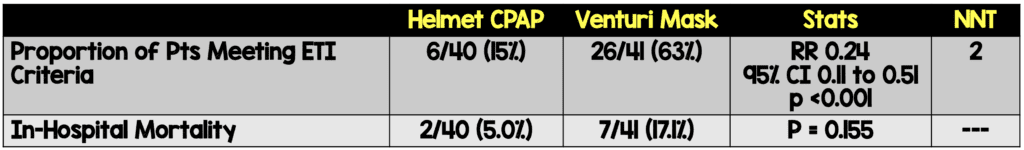
- In both groups the main causes of meeting ETI criteria were persistence of respiratory distress, reduction of at least 30% of baseline PaO2/FiO2 ratio, and SpO2 <90%
- 2 out of 6 patients meeting ETI criteria in the CPAP group did not tolerate the interface and required discontinuation of CPAP
- 2 patients in the CPAP group and 1 patient in the control group were intubated. The reason for the low number of intubations in the control group is that 18 patients were switched over to helmet CPAP (salvage therapy)
- In control group, mortality of patients receiving neither noninvasive or invasive ventilation was 2/5 (40%) vs 4/20 (20%) in patients treated with rescue noninvasive respiratory support
- Helmet CPAP showed a faster and greater improvement in oxygenation in comparison to controls (p <0.001)
- Hospital LOS did not differ between groups
- There was more discomfort to CPAP vs control however this was not statistically significant (15.0% vs 4.9%)
- No relevant adverse events in either group
Strengths:
- 1st randomized controlled trial evaluating helmet CPAP in patients with aHRF due to pneumonia
- Used an objective definition of pneumonia
- CXRs were evaluated by blinded radiologists
- Set objective clinical stability criteria
- All patients received their allocated intervention, none had the intervention discontinued, and zero patients were lost to follow up
- Severity of disease was fairly well balanced between groups (i.e. pneumonia severity index IV – V, CURB-65 ≥3, and respiratory distress)
- No protocol violations were seen in relation to inclusion or exclusion criteria
- Homogenous population of patients with pneumonia while excluding patients with hARF due to other concomitant causes
Limitations:
- Small number of patients may limit extrapolation to other clinical settings
- The primary outocome is subjective in nature and as clinicians are unblinded to intervention, bias could have affected the results
- It’s unclear why the comparison arm was Venturi masks as a non-rebreather can achieve better FiO2 (Possibly standard care in Italy?)
- Meeting objective criteria for intubation did not imply actual intubation, as the decision to intubate was left to physician discretion which could bias results. May have been better to have an outcome for escalation or change in O2 delivery as was shown in this trial
- Groups were not completely balanced at baseline with more patients in the control group actively smoking, more cardiovascular disease, COPD, and active cancer favouring the CPAP group (Almost 70% of patients meeting criteria for ETI)
- The primary outcome was criteria for ETI instead of mortality or intubation which are less subjective and better patient-oriented outcome
- Although ETI criteria were objectively defined, the recognition of exhaustion and respiratory distress could be seen differently based on physician assessment
- There is no data concerning the use of fluids and vasopressors in this study as both could cause major differences in outcomes (i.e. too much fluid)
- As with any new technology, there will be a learning curve to comfortably use and titrate helmet CPAP in settings not familiar with this
Discussion:
- The intubation rate in the control group was low, however this may be due to the fact that noninvasive respiratory support was used when intubation criteria were met. In fact this may be a proof of concept, when Venturi masks failed, physicians didn’t rush to intubate, they instead moved to NIV which was successful most of the time for salvage
- Although not statistically significant, patients treated with helmet CPAP had a mortality rate of 5% compared to the control group mortality of 40% in patients not receiving CPAP and 20% in patients treated with rescue noninvasive respiratory support
- A total of 6 patients felt uncomfortable with helmet CPAP in this study, but only 2 decided to interrupt treatment (2/40 = 5%)
Author Conclusion: “Helmet CPAP reduces the risk of meeting ETI criteria compared to oxygen therapy in patients with severe hARF due to pneumonia.”
Clinical Take Home Point: In this small RCT, evaluating a homogenous population of patients with pneumonia and hARF, helmet CPAP appears superior to standard oxygen therapy with Venturi mask in terms of ETI and a trend toward improved mortality.
Again, reached out to a good friend, and ED physician in Bergamo, Italy…Roberto Cosentini, MD (Who happens to be the final author on the paper we reviewed above). His thoughts are below:
Expert Opinion
Roberto Cosentini
Head Centro EAS Director – ASST Papa Giovanni XXIII – Bergamo, Italy
ASST Papa Giovanni XXIII – Bergamo, Italy
Milan, Italy
Twitter: @rob_cosentini
COVID19 Update with Helmet CPAP
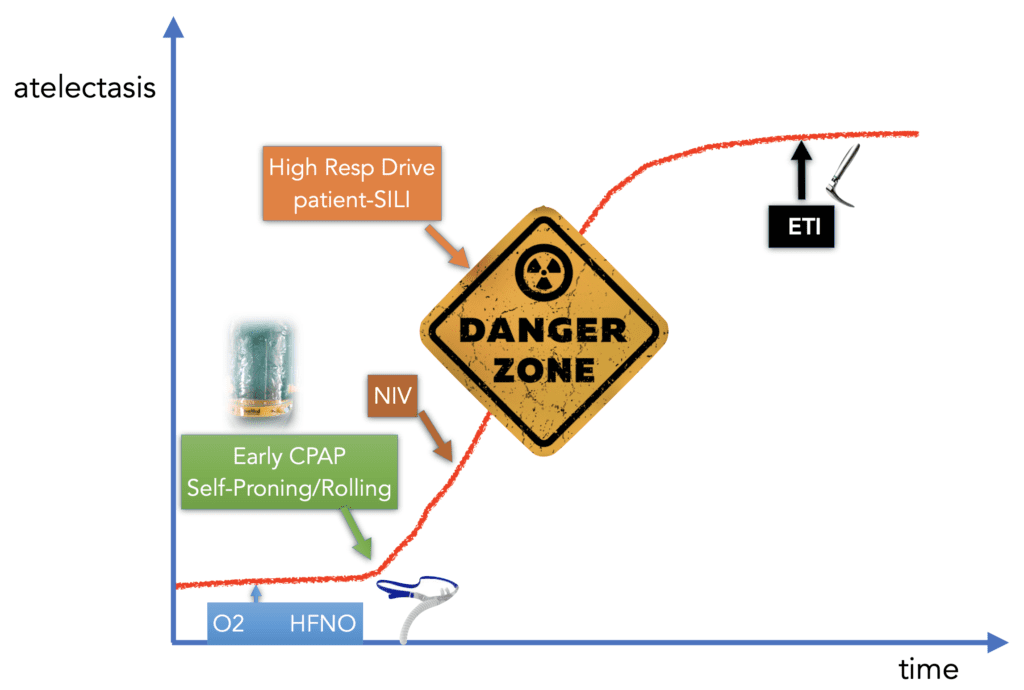
Roberto wanted to give credit to Josh Farkas for this modified graph
-
Is Helmet CPAP effective in COVID-19?
- We don’t know yet. We only have the Italian experience, and no RCTs
- The above RCT could be a proof of concept of Helmet CPAP as a means of oxygenation via alveolar recruitment in COVID-19 pneumonia
- In our experience, Helmet CPAP was applied in 198/508 COVID-19 hospitalized patients during the first 3 weeks of the Bergamo outbreak with a median P/F ratio of 180 and a mortality rate of 49% (DiMarco F et al…paper submitted for publication)
- Helmet CPAP alone allowed survival without ETI or ICU admission in 48/198 patients (47%)
-
Possible Advantages/Disadvantages?
- Efficacy:
- Pro: Improves oxygenation via alveolar recruitment
- Con: Reduces CO2, especially when lung compliance is normal
- Safety:
- Pro: No leaks, lower contamination risk, and better tolerance compared to other NIV interfaces and modalities
- Efficacy:
- One hypothesis on Helmet CPAP yet to be proven in a COVID-19 RCT, would be either early application to prevent ETI, or late as a bridge to ETI/ICU in cases of a new surge with limited resources
References:
- Brambilla AM et al. Helmet CPAP vs. Oxygen Therapy in Severe Hypoxemic Respiratory Failure Due to Pneumonia. Intensive Care Med 2014. PMID: 24817030
- Cosentini R et al. Helmet Continuous Positive Airway Pressure vs Oxygen Therapy to Improve Oxygenation in Community-Acquired Pneujonia: A Randomized, controlled Trial. PMID: 20154071
- Chidini G et al. Continuous Positive Airway Pressure with Helmet Versus Mask in Infants with Bronchiolitis: An RCT. Pediatrics 2015. [Epub Ahead of Print]
- Chidini G et al. Noninvasive Continuous Positive Airway Pressure in Acue Respiratory Failure: Helmet Versus Facial Mask. PMID: 20660548
For More Thoughts on This Topic Checkout:
- REBEL EM: COVID-19 NIV – Helmet vs Mask
Post Peer Reviewed By: Anand Swaminathan, MD (Twitter: @EMSwami)
The post Helmet CPAP vs Venturi Mask in Severe Acute Hypoxemic Respiratory Failure due to Pneumonia appeared first on REBEL EM - Emergency Medicine Blog.

