
 Take Home Points
Take Home Points
- Forget the “traditional” needle decompression landmark
- Decompress at 4th or 5th intercostal space in the anterior axillary line
REBEL Core Cast 32.0 – Needle Decompression
Diagnosis
- Tension pneumothorax is a clinical diagnosis
- Expect the pathology in a patient with chest injury, hypotension, unilateral breath sounds, tracheal deviation, hypotension and potentially hypoxia
- Physical exam, however, is unreliable
2015 meta-analysis archives of surgery
- <66% of patients had diminished breath sounds on the same side as lung collapse
- 10% of patients had diminished breath sounds on the opposite side of lung collapse
-
Classic findings, as usual, are actually uncommon
- Tracheal deviation and hypotension occurred in less than 1 in 5 patients
- Hypoxia occurred in less than 1 in 10 patients
- JVD occurred in less than 1 in 20 patients
Ultrasound (REBEL EM Link)
- Lung sliding is absent in collapsed lung
- M mode findings
- Seashore appearance in normal lung – subcutaneous tissue resembles the sea and normal lung resembles the sand
- In pneumothorax has barcode appearance, due to absence of lung movement
Literature Review 2010 Academic Emergency Medicine
- CXR v. US
- US sensitivity 86-90% & specificity of 97-100%
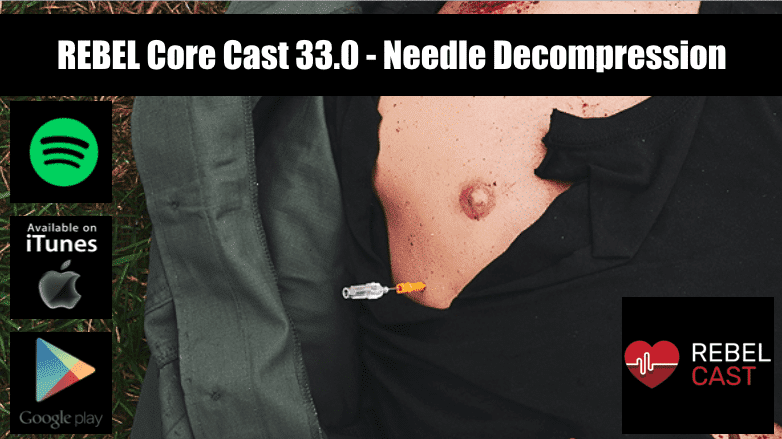
Treatment: Needle decompression
-
Traditional Approach
- 2nd intercostal space in the midclavicular line
- Difficulty finding the correct anatomical site, often times going too medially
- 14g angiocath (with 5cm length) will fail to reach the chest cavity in more than 50% of cases
-
Modern Approach
- 4th or 5th intercostal space in the anterior axillary line
- Chest wall is thinner making it easier to reach chest cavity
- Less vital structures that could be injured
- Easier to identify correct anatomical landmarks
Needle Catheter Dislodgement & Dysfunction
- Often times decompression done in the field and with repeated moves needle catheter can become dislodged
- Angiocath is also prone to kinking, plastic catheter becomes softer at body temperature and can kink when needle removed.
- Journal of Trauma and Acute Care surgery 2012 showed needle decompression failed 20% of the time due to kinking and dislodgement
Military Guidelines 2018
- Recommend needle decompression with 10g, 8cm angiocath angled perpendicular to the skin
- Hubbing catheter to the skin, and holding the entire needle/catheter unit in place for 5-10 seconds to improve decompression.
Finger Thoracostomy
- In crashing tension pneumothorax patient the most important thing is getting access to the chest cavity and guaranteeing decompression of tension pneumothorax
- May have less cognitive load burden secondary to just having to use a knife and finger
- Additionally in these cases will need to follow up with a chest tube so easy enough to finger decompress than follow it up with a chest tube
Take-Home Points
- Forget the “traditional” needle decompression landmark
- Decompress at 4th or 5th intercostal space in the anterior axillary line
More on the Topic
-
REBEL EM: Ultrasound Detection Pneumothorax
-
Taming the SRU: Needle Thoracostomy
- REBEL EM: What is the best anatomical position for needle thoracostomy
- EM Docs: Pneumothorax
Shownotes Written By: Miguel Reyes, MD (Twitter: @miguel_reyesMD)
Post Peer Reviewed By: Salim R. Rezaie, MD (Twitter: @srrezaie)
The post REBEL Core Cast 33.0 – Needle Decompression appeared first on REBEL EM - Emergency Medicine Blog.
