
 Every now and again someone raises the issue on social media about resuscitative thoracotomy. What are the indications (we have the EAST guidelines for that), what are the risks (highlighted in this important recent paper), and of course, whether EM or surgery should be doing it in the trauma bay (guess what – it’s in the curriculum for both specialties).
Every now and again someone raises the issue on social media about resuscitative thoracotomy. What are the indications (we have the EAST guidelines for that), what are the risks (highlighted in this important recent paper), and of course, whether EM or surgery should be doing it in the trauma bay (guess what – it’s in the curriculum for both specialties).
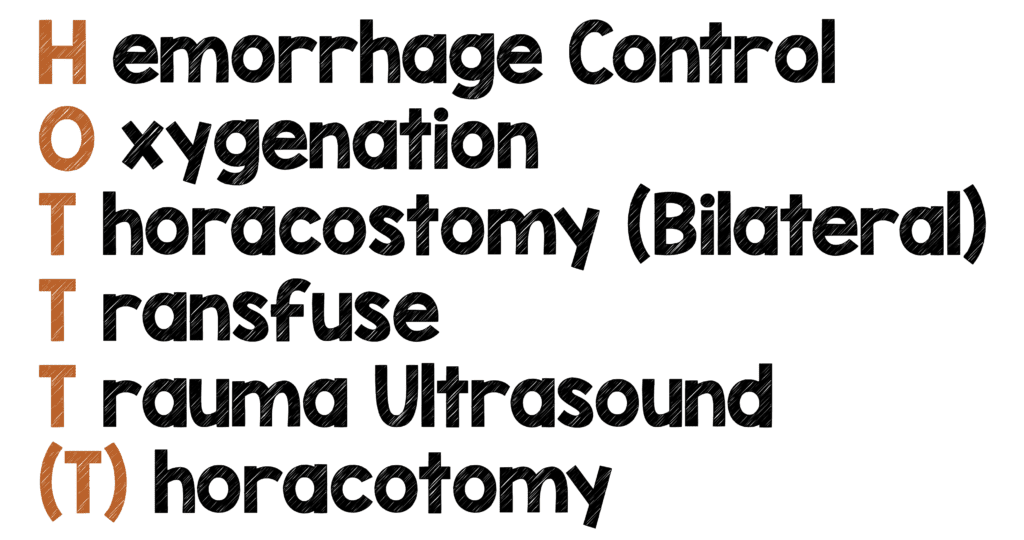
That’s not the point of this post. This post is about how I think you, as the emergency medicine physician (EP), working in a system where your surgeon is not in-house, but is available in a reasonable amount of time, should proceed when faced with the patient who meets the indications. You’ve gone through your HOTTT(T) algorithm and are now at that final “T” – you have to open the chest.
I think the technique you use is important. As an EP, a thoracotomy is an infrequent event that is an extremely high-adrenaline, high cognitive load situation and hence you should give yourself (and importantly your patient) the best chance to see and fix what you can. And that means doing a clamshell thoracotomy.
Clamshell you say?
The clamshell thoracotomy involves an incision extending across the entire anterior chest (mirroring the one made for the usual left anterolateral thoracotomy). After incising through the subcutaneous tissues, intercostal muscles, and sternum, the chest wall is lifted up (like opening a clamshell) allowing exposure to the intrathoracic organs and vessels.
The teaching is to proceed to a clamshell if you suspect a right-chest injury. So why am I advocating for this as an emergency physician? The exposure. While the left anterolateral approach is the most common used technique in the US (and this is acceptable), the view you get is limited and access to all important pathology can be difficult for those who don’t operate on chests on a regular basis.
When you are doing this for the first or second time in your career, you need to be able to see what you need to see, and the clamshell affords you much better exposure of the things you can possibly intervene on than a left anterolateral approach.
But time is of the essence!
The key to managing traumatic arrest is speed – the longer the duration of arrest, the worse the outcome, right? So, it goes to reason that opening the whole chest (clamshell) would take twice as long as opening half of it.
Maybe not. Two studies have compared the time to open the chest comparing the two techniques and found it took surgical and non-surgical clinicians the same time to perform both procedures. Control of a simulated wound was in fact shown to be subjectively easier and faster when the clamshell incision was used.
So what do I do next?
Let’s take a step back – as I mentioned there is a potential risk to the proceduralist whilst doing this procedure, so please ensure you are wearing appropriate personal protective equipment.
I am also a big advocate of having a simplified ED-specific thoracotomy tray if possible in your resuscitation room. The traditional sets picked up from the OR are too cumbersome and cause unnecessary confusion (and delay) when opened. Talk to the people responsible for providing sterile supplies in your hospital – you may be able to develop a simpler tray that is not going to add to your cognitive load when it is opened.
OK I’m ready…let’s go (step by step)
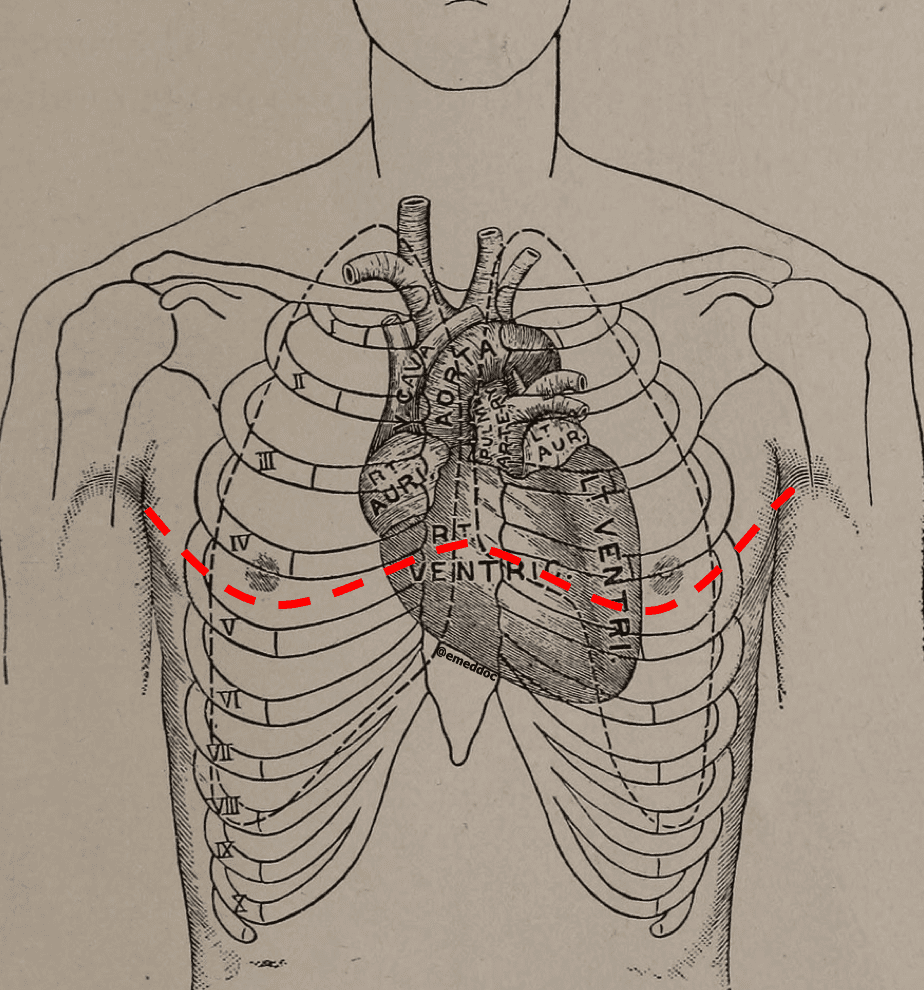
- As part of your trauma arrest algorithm, the patient should have been intubated and have had bilateral thoracostomies (in the 4th or 5th intercostal space, mid-axillary line) by now. If there is no return of circulation, and you have the right patient, the right indication, the right system, and the right tools, it’s time to open the chest.
- Remember, as this is a crash procedure, full sterility is not a priority – in fact the act of throwing betadine over the chest will probably just make things more slippery for you.
- Using a 10-blade scalpel, connect the bilateral thoracostomies. Make your incision count; cut through the skin and subcutaneous tissue down to the intercostal muscles. Try and remain in a single intercostal space. You may need to extend the incision laterally, but if you do so, remember to not go straight down to the bed, but extend up into the axillae.
- Using heavy scissors, cut through the intercostal muscles towards the sternum. In order to protect the lung, I’ll usually put initially two fingers and then my hand into the incision, pushing the lung away whilst cutting over my hand.
- The sternum is the next structure to get through – you can use heavy scissors, trauma shears, a Lebsche knife, or a Gigli saw. I think the first two are much more familiar to the emergency physician and pretty effective. You’ll also be cutting through the inferior mammary arteries when you do this, but you can deal with those after you’ve restored circulation.
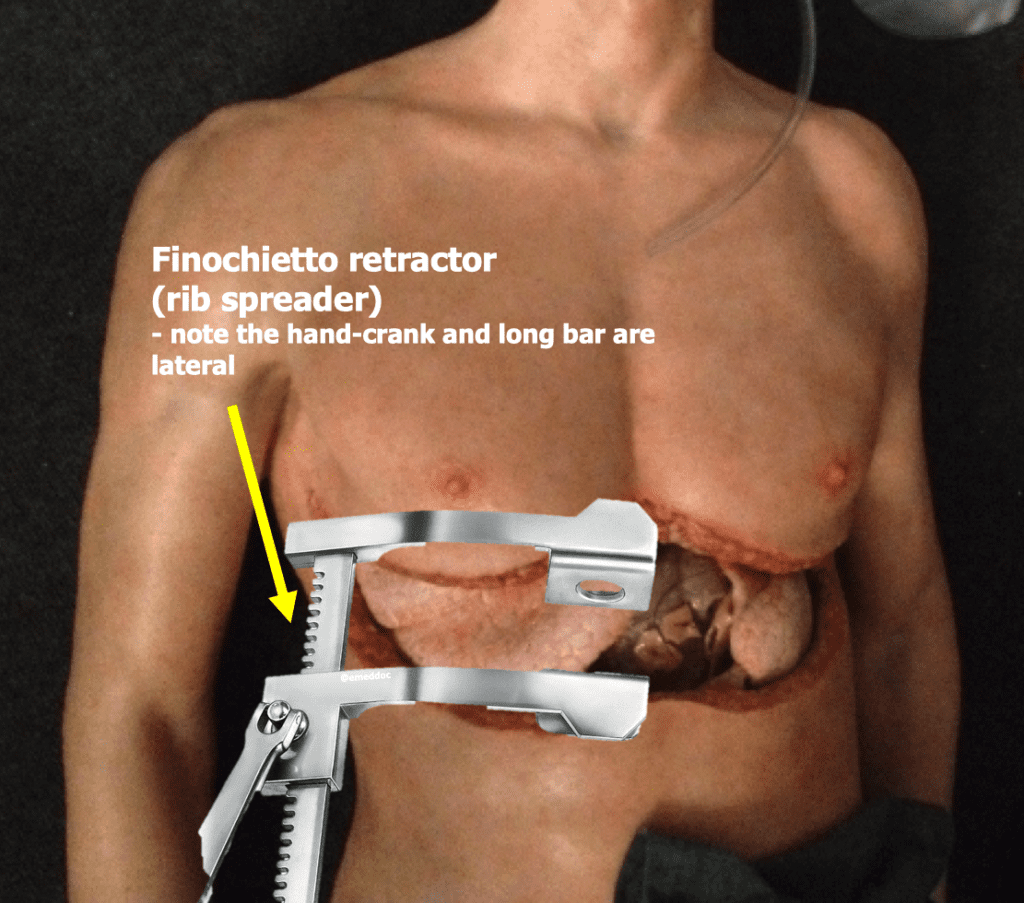
- Now that you are through the sternum, lift up the chest wall (clamshell) and expose the thoracic organs. Place your rib-spreader so it’s not in your way (the hand-crank and long metal bar should be lateral) and open the cavity wider. There is often some fibrous tissue between the anterior aspect of the pericardium and the posterior sternum which you should divide with scissors.
What are my priorities now?
Once the chest is open, your priorities as an emergency physician are:
- Open the pericardium to relieve tamponade
- Identify and repair any cardiac injuries
- Perform internal cardiac compressions
- Cross-clamp the aorta if needed
- In the presence of major lung injury, collapse and compress the lung
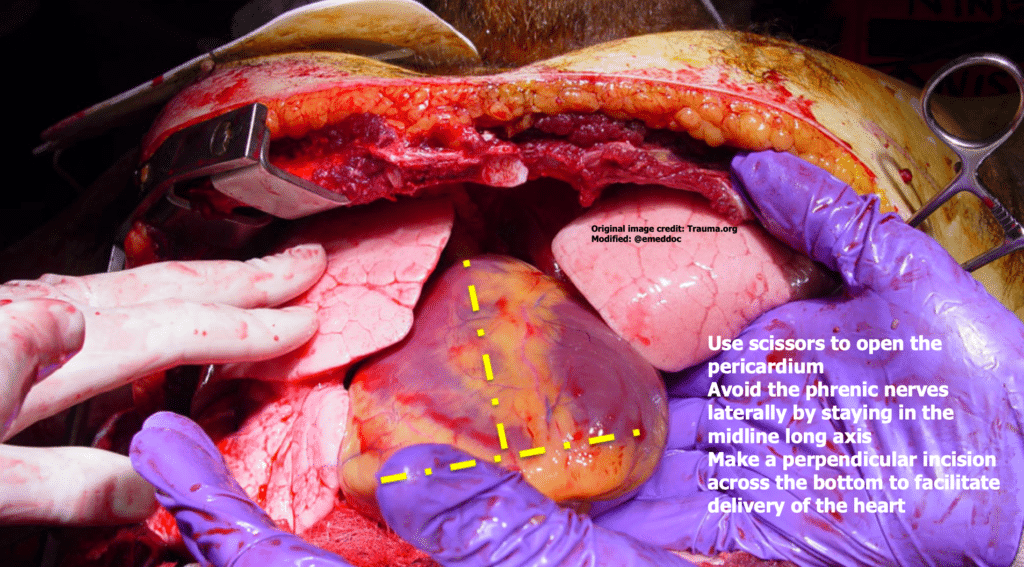
- Always open the pericardium – even if you’re not sure there’s tamponade. A small amount of blood accumulating rapidly in that tight space can lead to tamponade. While you can use forceps to pick up the pericardium in the anterior midline, sometimes it can be very tense and difficult to grasp. I make an upside-down T-shaped incision, with the long stem in the mid long axis, and the shorter segment across the bottom – this stays away from those phrenic nerves running down either side of the pericardium and opens it up enough for you to evacuate any blood and then deliver the heart.
- Look at all heart’s surfaces (including the back) rapidly for any wounds that can be closed – more on this later.
- Internal compressions rely on you moving blood from the apex to the aorta – a hand should be placed on either surface and the heart is squeezed from the apex upwards. Make sure you allow the heart to fill in between beats – this can be impaired if you do not keep the heart horizontal. Flicking the heart can sometimes coax it into beating.
- You may need to cross-clamp the aorta – the intent being to redirect blood to improve cardiocerebral perfusion. This is best done just above the diaphragm, and involves incising through the inferior pulmonary ligament, bluntly dissecting down to separate the aorta from the esophagus, and placing a vascular (Satinsky) clamp. It is challenging in a pulseless patient to differentiate the two tubes, and so have someone drop an orogastric tube down to help you identify the esophagus. Again, if you’ve not had to do this before, it becomes that much more challenging, so a temporary solution would be to have an assistant compress the distal thoracic aorta against the vertebral column with their hand.
- Internal paddles will be needed if the heart is fibrillating – start with a 10-20J (and use the same precautions as you would use with external defibrillation).
But what about those holes?
Wounds to the myocardium can be addressed in a number of ways:
- Put a finger on it – especially if it’s small
- Use staples – a standard skin stapler can be very effective in temporarily closing wounds
- Suture the wounds – use a large size but be very careful not to inadvertently tie off a coronary vessel
I do not advocate placing a Foley in the wound. This used to be advised, but it is problematic for a number of reasons. The tension applied to the balloon can actually cause it to rip through the myocardium, causing even more damage. Additionally, the cardiac chambers aren’t that big to begin with, and you may inadvertently reduce the chamber volume even further by having the balloon there, thus reducing ventricular filling and hence cardiac output.
Finally, in the setting of a unilateral lung injury that may have caused a massive hemothorax, be careful about clamping the hilum or twisting the lung. Both can be difficult to do. Rather, you can compress down the entire lung onto the hilum. This may provide temporary control.
Final Thoughts
The end-point, ideally, is ROSC, when a few things may happen. The patient may wake up and so will require appropriate sedation. The internal mammary arteries may start bleeding and should be controlled with hemostats or tied off. Remember – you need to have a plan to get the patient expediently to surgical care and resuscitation should remain ongoing.
Even if you do not achieve ROSC, at least you will know that when the decision was made to proceed with thoracotomy, you did the best you could for the patient.
References:
- Seamon MJ, et al. An evidence-based approach to patient selection for emergency department thoracotomy: A practice management guideline from the Eastern Association of Trauma. J Trauma Acute Care Surg 2015:159-173 PMID: 26091330
- Nunn A, et al. Occupational exposure during emergency department thoracotomy: A prospective multi-instituion study. J Trauma Acute Care Surg 2018. PMID: 29664893
- American Board of Emergency Medicine’s 2016 Model of the Clinical Practice of Emergency Medicine. Link
- American Board of Surgery Curriculum Outline for General Surgery 2018-2019 Link
- Puchwein P, et al. Clamshell thoracotomy and open-heart massage-a potential life-saving procedure can be taught to emergency physicians: An educational cadaveric pilot study. Injury 2015:1738-1742 PMID: 26068645
- Flaris AN, et al. Clamshell incision versus left anterolateral thoracotomy: Which one is faster when performing a resuscitative thoracotomy? The tortoise and the hare revisited. World J Surg 2015:1306-1311 PMID: 25561192
-
Weingart S. The abbreviated ED thoracotomy tray. EMCritt RACC blog 2015. [Link]
Post Peer Reviewed By: Anand Swaminathan, MD (Twitter: @EMSwami) and Salim R. Rezaie, MD (Twitter: @srrezaie)
The post If You’re Going to do the Thoracotomy…do a Clamshell appeared first on REBEL EM - Emergency Medicine Blog.
