
 This years ACEP 2016 conference took place in Las Vegas, NV from Oct 16th – 19th. There was greater than 350 courses, labs, and workshops given throughout the week. It was impossible to make all of these great lectures, but I was able to take away some very important clinical pearls that I wanted to share with our readers.
This years ACEP 2016 conference took place in Las Vegas, NV from Oct 16th – 19th. There was greater than 350 courses, labs, and workshops given throughout the week. It was impossible to make all of these great lectures, but I was able to take away some very important clinical pearls that I wanted to share with our readers.
Clinical Pearls from ACEP 2016
What are some of the Interventions in EM that Matter (The Number Needed to Treat)?
- The Number Needed to Treat (NNT) = 1/Absolute Risk Reduction(ARR)
- The Smaller the NNT the Bigger the Impact
- ARR of 50% Gives you a NNT = 2
- ARR of 25% Gives you a NNT = 4
- ARR of 5% Gives you a NNT = 20
- ARR of 2% Gives you a NNT = 50
- ASA in STEMI to Save a Life: NNT = 42
- Clopidogrel After MI or PCI to Prevent Another MI or Stroke: NNT = 27
-
Steroids for Asthma
- To Prevent Hospital Admission: NNT = 8
- To Prevent Asthma Recurrence: NNT = 10
- Cyclobenzaprine (Flexeril) for Back Pain
- Medication Side Effects: NNH = 4
- Global Improvement of Pain at 10 Days: NNT = 3
- Ibuprofen for Tension Type Headaches
- Pain Free at 2 Hours: NNT = 14
- Not Taking Rescue Medication: NNT = 9
- Improvement in Pain Scale Rating: NNT = 6
- Gabapentin for Neuropathic Pain
- Diabetic Neuropathy: NNT = 6
- Herpetic Neuralgia: NNT = 8
- Ataxia: NNH = 13
- Somnolence: NNH = 11
- Dizziness: NNH = 8
- Erythromycin or Reglan Before Endoscopy to Avoid Repeat Endoscopy: NNT = 9
- Octreotide for Variceal Bleeding
- Improvement in Mortality or Rebleeding: NNT = Infinity (No Benefit)
- Octreotide does decrease blood transfusion by average of 0.7 Units of PRBCs
- Antibiotics in Cirrhotics with UGIB
- Mortality: NNT = 25
- Infection Prevention: NNT = 4
- PPIs for UGIB after EGD
- Rebleeding: NNT = 15
- Avoid Surgery: NNT = 33
- No Difference in Mortality unless Asian Descent: NNT = 33
- PPIs Before EGD
- Mortality, Transfusion, Hospital Stay, and Surgery: NNT = Infinity (No Benefit)
- Avoid Intervention During EGD: NNT = 33
- Conservative Transfusion Threshold in UGIB
- Mortality: NNT = 25
- Avoid Transfusion Reaction: NNT = 13
- Antibiotics for Sinusitis
- Side Effects: NNH = 8
- Faster Symptom Resolution: NNT = 18
- Antibiotics for Otitis Media
- Disease Recurrence: NNT = Infinity (No Benefit)
- Serious Complications or Pain at 24 Hours: NNT = Infinity (No Benefit)
- Pain Reduction at Days 2 – 7: NNT = 20
- Diarrhea: NNH = 9
- Tranexamic Acid (TXA) in Trauma Patients with Suspected Bleeding
- Mortality: NNT = 67
- Steroids or Pneumonia
- Avoid Intubation: NNT = 20
- Prevent ARDS: NNT = 16
- Hyperglycemia: NNH = 29
What Were Some of the Big Papers Discussed for Trauma?
- REACT 2 Trial [4]: Immediate Total-Body CT scanning of trauma patients DOES NOT reduce in-hospital mortality compared with selective radiological work-ups
- NEXUS Chest CT Rule Trial [5]: Using a clinical decision instrument in patients with blunt trauma can safely reduce unnecessary chest CTs by 25 – 37%
- PROPPR Trial [6]: In trauma patients requiring massive transfusion protocols, transfusion in a 1:1:1 ratio of platelets, plasma, and red blood cells seems to decrease death from exsanguination at 24 hours and achieves more rapid hemostatsis
-
Tranexamic Acid (TXA) to Trauma Patients who we Think are Bleeding
- MATTERs Trial [1]:
- Unadjusted Mortality: 17.4% TXA vs 23.9% no TXA
- Greatest Benefit in Patients with Massive Transfusion: 14.4% TXA vs 28.1% no TXA
- MATTERs II Trial [2]:
- Mortality: 11.6% TXA/Cryoprecipitate vs 18.2% TXA vs 21.4% Cryoprecipitate vs 23.6% no TXA/Cryoprecipitate
- CRASH-2 Trial [3]:
- All -Cause Mortality: 14.5% TXA vs 16.0% Placebo
- CLINICAL BOTTOM LINE: In Trauma patients who you think are bleeding give 1g TXA IV followed by 1g given as an infusion over the next 8 hours. The biggest impact is seen in patients given TXA <1hrs from injury and patients requiring massive transfusion protocols
- MATTERs Trial [1]:
What Were Some of the Big Papers Discussed for Critical Care?
- INTERACT II [7] & ATACH-2 [8]: Aggressive Lowering of Blood Pressure (<140mmHg) in Early Ischemic Stroke has NO Significant Beneficial or Negative Effects on Death/Dependency.
- PATCH Trial [9]: Platelet transfusion should be avoided in patients with an ICH taking anti platelet therapy (Applies to patients NOT having a neurosurgical procedure)
- VL vs DL during CPR [10]: It is more common to have significant interruptions of compressions with DL
- ALPS Trial [11]: Both amiodarone and lidocaine showed similar benefits with respect to short-term outcomes in OHCA due to initial shock refractory ventricular fibrillation or pulseless ventricular tachycardia compared to placebo, but this did not result in a higher rate of survival to hospital discharge or favorable neurologic outcomes. In a subgroup analysis, amiodarone and lidocaine had a higher rate of survival to hospital discharge than placebo among patients with witnessed OHCA
- Prognostication in Post Cardiac Arrest Patients [12]: Do not use the ED neurological exam to guide care/counsel to family on possible outcomes in patients who are post cardiac arrest who are undergoing therapeutic hypothermia
- Sepsis 3.0 [13]: SIRS has been replaced by qSOFA and SOFA for mortality prediction in sepsis. However we are giving up sensitivity to increase specificity. Recently, qSOFA was compared to SIRS and other early warning scores [14] showing that commonly used early warning scores are more accurate than qSOFA for predicting death and ICU transfer
What Were Some of the Big Papers Discussed for ECGs?
-
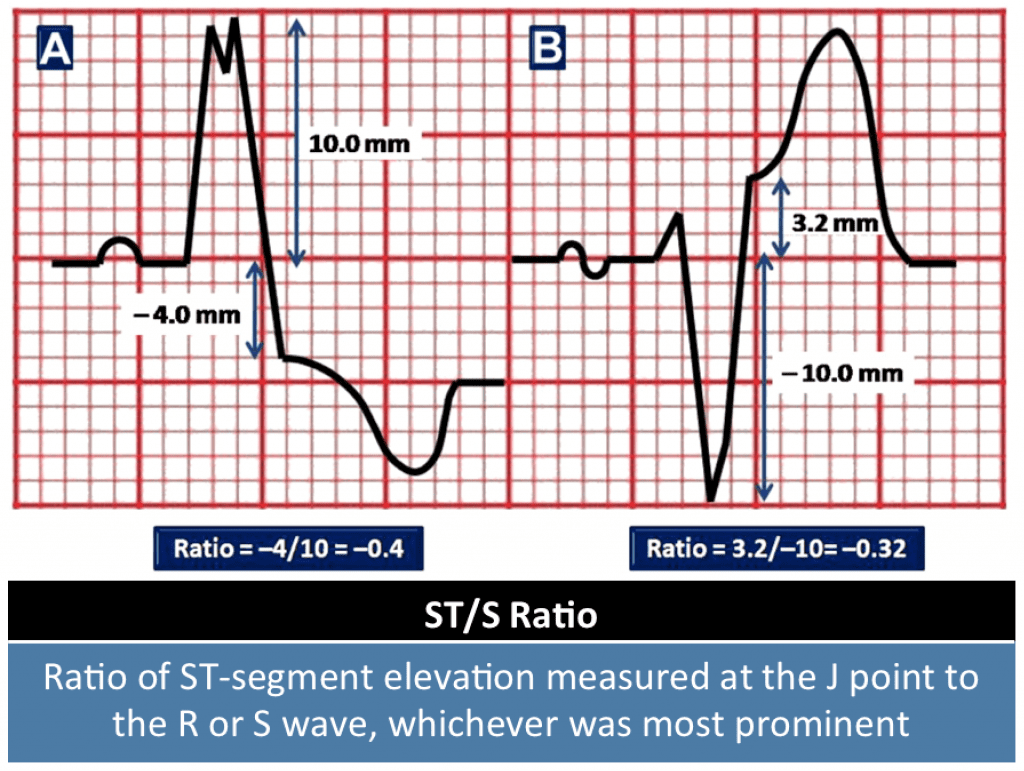
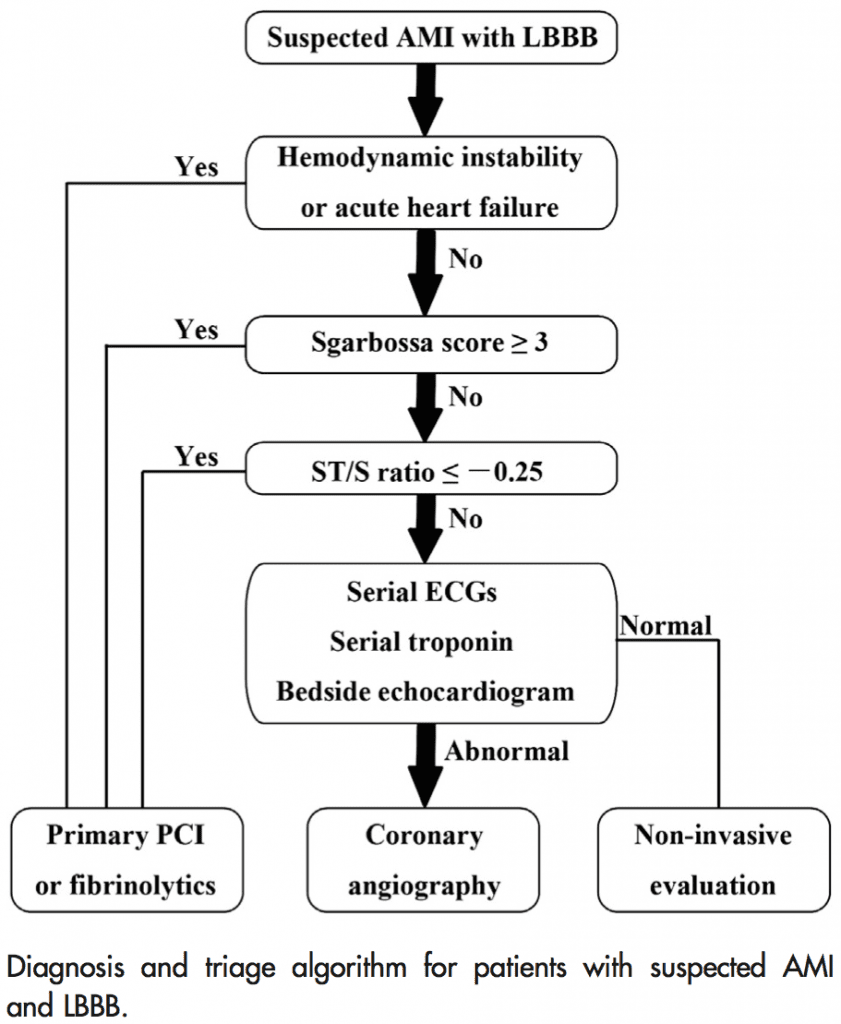
Modified Sgarbossa Criteria [15] [16]:
- It is still possible to identify STEMI in the setting of LBBB using the modified Sgarbossa Criteria:
- Concordant ST-Segment Elevation ≥1mm in Any Lead
- Concordant ST-Segment Depression ≥1mm in Lead V1 – V3
- Discordant ST/S Ratio ≤-0.25
- It is still possible to identify STEMI in the setting of LBBB using the modified Sgarbossa Criteria:
-
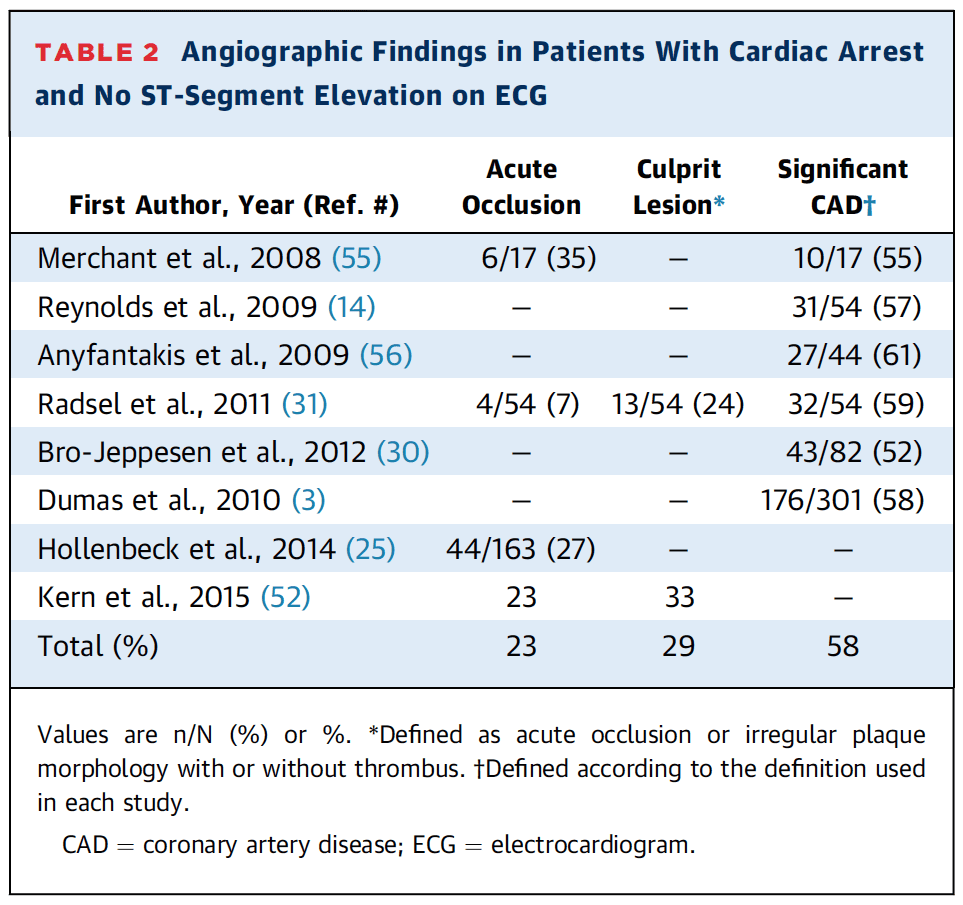
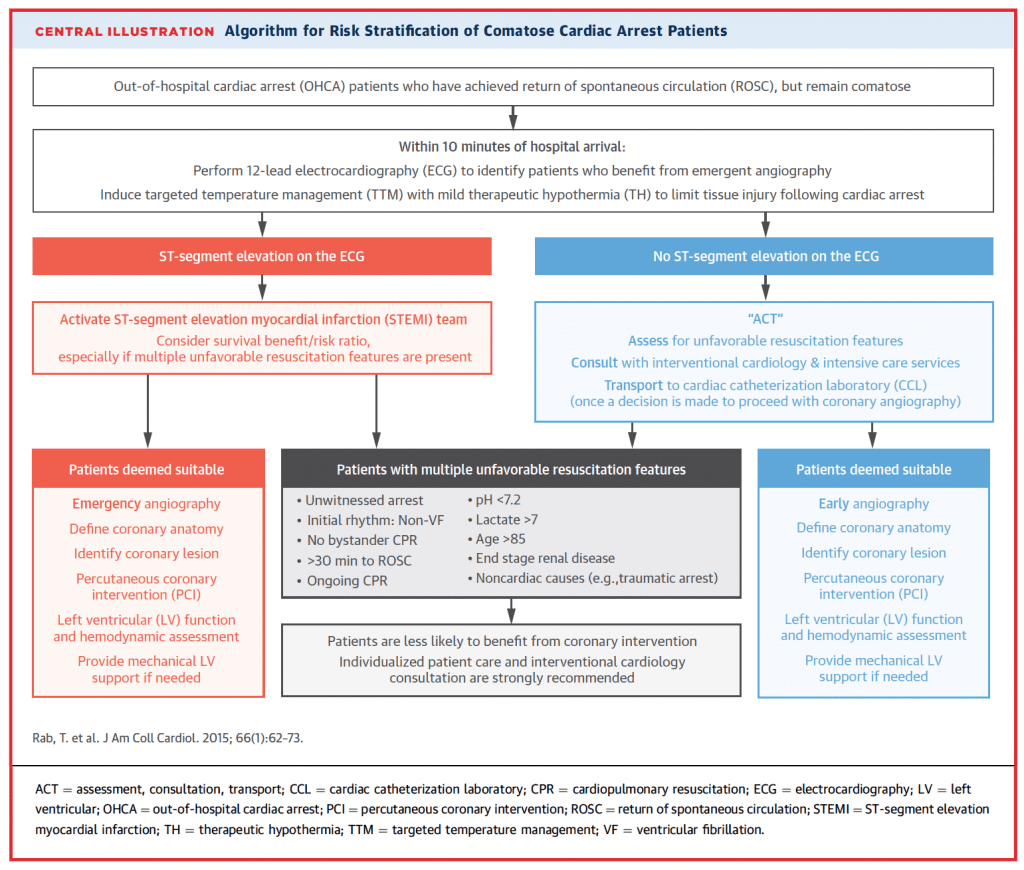
Post Arrest Patients with Non-STEMI [17]:
- The majority of patients with ROSC after cardiac arrest do not have ST-Segment Elevation on post-arrest ECG. 1/4 of these patients will have an acute coronary occlusion and nearly 60% will have significant obstructive lesions.
-
Benign Early Repolarization vs STEMI [18]:
- (1.196 x STE at 60ms after the J-Point in V3 in mm) + (0.059 x computerized QTc) – (0.326 x R-Wave Amplitude in V4 in mm)
- A Value >23.4 is quite sensitive and specific for LAD Occlusion
- Calculator for this HERE
References:
- Morrison JJ et al. Military Application of Tranexamic Acid in Trauma Emergency Resuscitation (MATTERs) Study. Arch Surg 2012; 147(2): 113 – 9. PMID: 22oo6852
- Morrison JJ et al. Association of Cryoprecipitate and Tranexamic Acid with Improved Survival Following Wartime Injury: Findings from the MATTERs II Study. JAMA Surg 2013; 148(3): 218 – 25. PMID: 23670117
- CRASH-2 Trial Collaborators. Effects of Tranexamic Acid on Death, Vascular Occlusive Events, and Blood Transfusion in Trauma Patients with Significant Hemorrhage (CRASH-2): A Randomized, Placebo-Controlled Trial. Lancet 2010; 376(9734): 23 – 32. PMID: 20554319
- Siring JC et al. Immediate Total-Body CT Scanning Versus Conventional Imaging and Selective CT Scanning in Patients with Severe Trauma (REACT-2): A Randomized Controlled Trial. Lancet 2016; 388(10045): 673 – 83. PMID: 27371185
- Rodriguez RM et al. Derivation and Validation of Two Decision Instruments for Selective Chest CT in Blunt Trauma: A Multicenter Prospective Observational Study (NEXUS Chest CT). PLoS Med 2015; 12(10). PMCID: PMC 4595216
- Holcomb JB et al. Transfusion of Plasma, Platelets, and Red Blood Cells in a 1:1:1 vs a 1:1:2 Ratio and Mortality in Patients with Severe Trauma: The PROPPR Randomized clinical Trial. JAMA 2015; 313 (5): 471 – 82. PMID: 25647203
- Anderson CS et al. Rapid Blood-Pressure Lowering in Patients with acute Intracerebral Hemorrhage. NEJM 2013; 368(25): 2355 – 65. PMID: 23713578
- Qureshi Al et al. Intensive Blood-Pressure Lowering in Patients with Acute Cerebral Hemorrhage. NEJM 2016; 375 (11): 1033 – 43. PMID: 27276234
- Baharoglu MI et al. Platelet Transfusion Versus Standard Card After Acute Stroke due to Spontaneous Cerebral Hemorrhage Associated with Antiplatelet Therapy (PATCH): A Randomized, Open-Label, Phase 3 Trial. Lancet 2016; 387(10038): 2605 – 13. PMID: 27178479
- Kim JW et al. Video Laryngoscopy vs Direct Laryngoscopy: Which Should be Chosen for Endotracheal Intubation During Cardiopulmonary Resuscitation? A Prospective Randomized Controlled Study of Experienced Intubators. Resuscitation 2016; 105: 196 – 202. PMID: 27095126
- Kudenchuk PJ et al. Amiodarone, Lidocaine, or Placebo in Out-of-Hospital Cardiac Arrest. NEJM 2016; 374(18): 1711 – 22. PMID: 27043165
- Merrill et al. Early Neurologic Examination is not Reliable for Prognostication in Post-Cardiac arrest patients who undergo Therapeutic Hypothermia. Am J Emerg Med 2016; 34(6): 975 – 9. PMID: 26994681
- Singer M et al. The Third International consensus Definitions for Sepsis and Septic Shock (Sepsis-3). JAMA 2016; 315(8): 801 – 10. PMID: 26903338
- Churpek MM et al. qSOFA, SIRS, and Early Warning Socres for Detecting Clinical Deterioration in Infected Patients Outside the ICU. Am J Respire Cirt Care Med 2016. [ePub Ahead of Print] PMID: 27649072
- Smith SW et al. Diagnosis of ST-Elevation Myocardial Infarction in the Presence of Left Bundle Branch Block with the ST-Elevation to S-Wave Ratio in a Modified Sgarbossa Rule. Ann Emerg Med 2012; 60(6): 766 – 76. PMID: 22939607
- Meyers HP et al. Validation of the Modified Sgarbossa Criteria for Acute Coronary Occlusion in the Setting of Left Bundle Branch Block: A Retrospective case-Control Study. AHJ 2015; 170(6): 1255 – 64. PMID: 26678648
- Rab T et al. Cardiac Arrest: A Treatment Algorithm for Emergent Invasive Cardiac Procedures in the Resuscitated Comatose Patient. J Am Coll Cardiol 2015; 66(1): 62 – 73. PMID: 26139060
- Smith SW et al. Electrocardiographic Differentiation of Early Repolarization from Subtle Anterior ST-Segment Elevation Myocardial Infarction. Ann Emerg Med 2012; 60(1): 45 – 56. PMID: 22520989
Post Peer Reviewed By: Anand Swaminathan (Twitter: @EMSwami)
The post American College of Emergency Physicians (ACEP) Conference 2016 appeared first on REBEL EM - Emergency Medicine Blog.
