
 This year ACEP 2017 took place in Washington D.C. from Oct. 29th – Nov 1st, 2017. There were lots of amazing speakers and topics as was evidenced by the eruption of everyone’s twitter feeds with the #ACEP17 hashtag. I was fortunate enough to attend this amazing conference and approached by several attendees if I would put together a list of my favorite pearls from this conference. I decided to put a top 10 list together, in no particular order.
This year ACEP 2017 took place in Washington D.C. from Oct. 29th – Nov 1st, 2017. There were lots of amazing speakers and topics as was evidenced by the eruption of everyone’s twitter feeds with the #ACEP17 hashtag. I was fortunate enough to attend this amazing conference and approached by several attendees if I would put together a list of my favorite pearls from this conference. I decided to put a top 10 list together, in no particular order.
Pearl #1: The Diagnostic Performance of Computer Programs for Interpretation of of ECGs[1]
- What They Did: Comparison of 9 ECG computer programs vs 8 cardiologists interpreting 1220 clinically validated cases of various cardiac disorders
- Control patients = 382
- LVH = 183
- RVH = 55
- Anterior MI = 170
- Inferior MI = 273
- Median Correct Diagnosis:
- Computer Programs: 91.3%
- Cardiologists 96.0%
- p < 0.01
- Median Sensitivity to Diagnose Anterior MI
- Computer Programs: 77.1%
- Cardiologists: 84.9%
- p < 0.01
- Median Sensitivity to Diagnose Inferior MI:
- Computer Programs: 58.8%
- Cardiologists 71.7%
- p < 0.001
- The median total accuracy level (percentage of correct classifications was 6.6% lower for computer programs than cardiologists (69.7% vs 76.3%)
- Study Bottom Line: Don’t rely on the computer for ECG interpretations
Pearl #2: Hyperkalemia is the “Syphilis” of ECGs [2]
- What They Did: Collected 188 ECGs of patients with severe hyperkalemia (K+ ≥6.5mEq/L)
- Adverse events occurred within 6 hours in 28 patients (15%)
- Symptomatic Bradycardia in 22 patients (12%)
- Death in 4 patients (2%)
- Ventricular Tachycardia in 2 patients (1%)
- CPR in 2 patients (1%)
- All adverse events occurred prior to treatment with calcium
- Most Common ECG Findings Predicting Adverse Outcomes:
- QRS prolongation 79%
- Bradycardia (HR <50 bpm) 61%
- PR Prolongation 50%
- Junctional Rhythm 39%
- Peaked T Waves 25%
- We have written about this before on REBEL EM: ECG Changes of Hyperkalemia
- Study Bottom Line: When ACLS is not working, think tox or hyperK+ (i.e. In a code situation, just give Calcium prior to K+ level as there is really no downside to doing this)
Pearl #3: Tidal Volume on the Ventilator is Based off IDEAL BODY WEIGHT not Actual Body Weight
- Lung Size for a 250lb and 100lb patient of the same height are essentially the same

- For a great resource on this checkout MDCalc: Endotracheal Tube (ETT) Depth and Tidal Volume Calculator
Pearl #4: If you Have a Critical Patient and Can’t Get IV Access Consider These Options [3] [4]
- What They Did: 16 Cadavers underwent a 5 minute bolus infusion of fluid via three IO access sites:
- Flow Rates:
- Sternum: 93.7 mL/min
- Proximal Humerus: 57.1mL/min
- Proximal Tibia: 30.7 mL/min
- Sternum access requires special IO needle not always available at institutions and could affect CPR quality
- Tibial Access had the greatest number of insertion difficulties
- Flow Rates:
- What They Did: Multicenter prospective observational trial to evaluate the efficacy and safety of the Easy IJ in 74 patients
- Initial Success Rate: 88%
- Mean Procedure Time: 4.4 min
- Number of Skin Punctures: 1 (75%), 2 (19%), 3 – 5 (6%)
- Complications: Pneumothorax, Line Infection, Arterial Puncture (0%); Loss of Patency (10/73 – 14%)
- We Have Written About This Before on REBEL EM: The Easy IJ – Another Option for Difficult IV access in Stable Patients?
- Study Bottom Line: If you are having difficulty getting IV access in your critically ill patient, consider, IO access Proximal Humerus > Proximal Tibia or the Easy IJ
Pearl #5: Nitroglycerin NOT Furosemide Should Be First-Line in Treatment of CHF and Pulmonary Edema
- The goals of treatment in cardiogenic pulmonary edema
- Decrease Preload
- Decrease Afterload
- Improve LV Function
- Initial treatment should therefore focus on fluid redistribution not fluid removal
- Morphine associated with increased intubation, Increased ICU admission, and Increased mortality; No role in treatment of cardiogenic pulmonary edema [5]
- Diuretics: Due to increased afterload, effects are often delayed 30 – 120 minutes; Not effective in anuric ESRD patients; May also decrease CO during first 90 minutes [6]
- Nitroglycerin: Rapid, reliable preload reduction and effective afterload reduction at higher doses, so be aggressive 100 – 400mcg/min [7]
- NIPPV; Decreases preload and afterload which help increase CO
- More than 50% of patients with cardiogenic pulmonary edema are euvolemic [8]
- Summary of Treatment Options in Cardiogenic Pulmonary Edema:
- NIVPPV – First line treatment
- Nitroglycerin – First line agent
- ACE-Inhibitors – Second line agent
- Furosemide – Third Line Agent
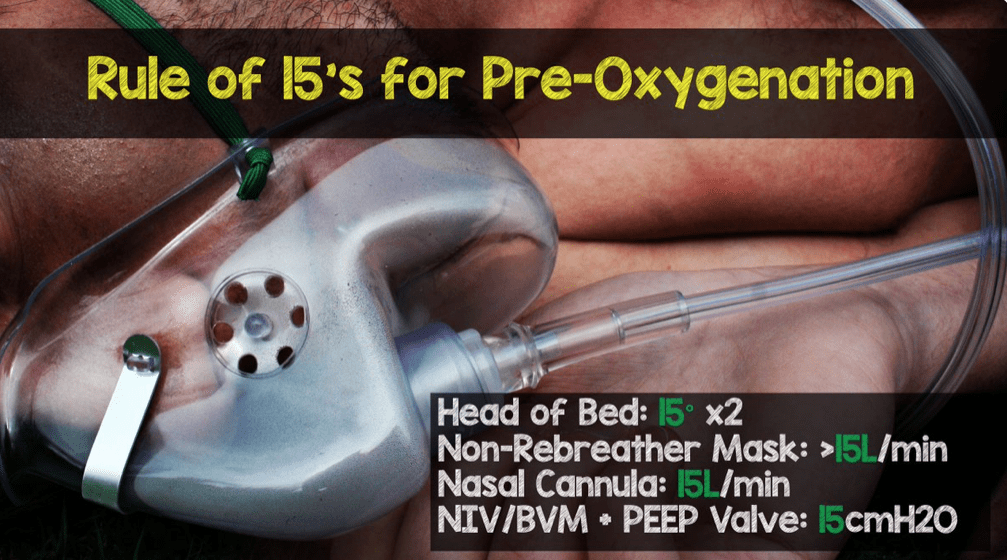
Pearl #6: Remember the Rule of 15’s for Pre-Oxygenation Prior to RSI to Prevent Oxygen Desaturation
- Back Up Head Elevated (BUHE) Intubation [9]:
- 528 Intubations
- Primary Outcome: Composite of Any Intubation Related Complication (Difficult Intubation ≥3 Attemps or >10 min, Hypoxemia <90% O2 Sat, Esophageal Intubation, or Esophageal Aspiration)
- Standard Supine Intubation: 22.6%
- BUHE Intubation 9.3%
- Flush Rate O2 for Pre-Oxygenation [10]:
- Crossover trial with healthy volunteers with:
- NRB at 15L/min (NRB-15)
- NRB with Flush Rate (>40L/min) O2 (NRB-Flush)
- BVM Device with O2 at 15L/min (BVM-15)
- Simple Mask with Flush Rate (>40L/min) O2 (SM-Flush)
- Forced Expiratory O2 in a single Exhaled Breath (FeO2) After 3 Min Pre-Oxygenation:
- NRB-15: 54%
- NRB-Flush: 86%
- BVM-15: 77%
- SM-Flush: 72%
- Crossover trial with healthy volunteers with:
- Apneic Oxygenation RCT in the ED [11]:
- Single Institution RCT of 200 patients randomized to Apneic Oxygenation vs No Apneic Oxygenation
- Lowest Mean O2 Saturation:
- Apneic Oxygenation: 92%
- Usual Care: 93%
- Caveats: 70% of patients intubated by 60 seconds, 80% by 80 seconds, 90% by 100 seconds, and 100% by 195 seconds
- All patients pre-oxygenated for ≥ 3minutes
- In patients with shunt physiology (Pneumonia, Pulmonary Edema, PE), remember that oxygenation will not help as much as PEEP (Recruit Atelectatic Alveoli)
- For all causes of hypoxia NC>15LPM + BVM 15LPM _ PEEP Valve 15cmH20 = Best PreOx, ApOx, and ReOx currently available
- Bottom Line of Studies:
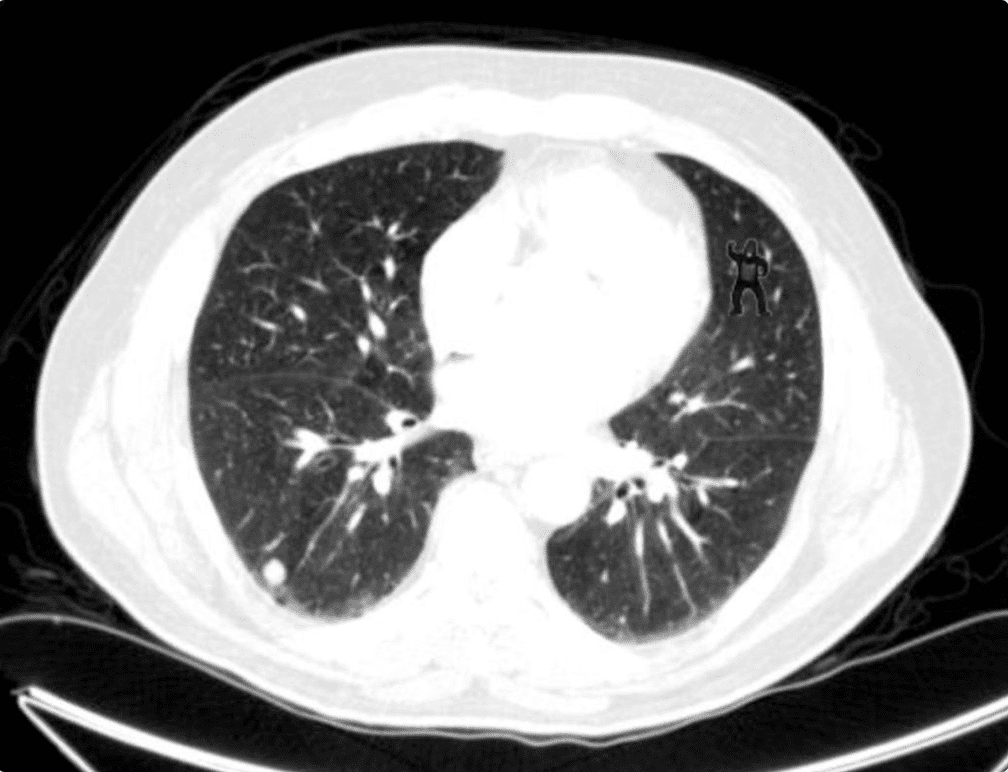
Pearl #7: Radiologists are NOT “All-Seeing” [12]
- “The Invisible Gorilla Strikes Again”
- 24 radiologists had up to 3 minutes to freely scroll through lung CTs searching for nodules
- A Small Gorilla was also superimposed on the CTs as an experiment of inattentional bias
- 20/24 (83%) radiologists failed to see the gorilla
- Study Bottom Line: ALWAYS look at all radiology images that you order and not just the radiology read
Pearl #8: NPO Status in Pediatric Patients Prior to Sedation/Anesthesia Outside the Operating Room [13]
- What They Did: Pediatric Sedation Research Consortium evaluated >139,000 procedural sedation/anesthesia encounters from 42 institutions
- Evaluated Aspiration Episodes and Composite Major Adverse Events (Aspiration, Death, Cardiac Arrest, Unplanned Hospital Admission) with respect to NPO status
- Aspiration:
- NPO = 8/82,546 (0.01%)
- Non-NPO = 2/25,401 (0.008%)
- Composite Major Adverse Events:
- NPO = 46/82,546 (0.06%)
- Non-NPO = 15/25,401 (0.06%)
- 0 Deaths
- Study Bottom Line: There is no association between NPO status and aspiration or composite major adverse events in sedation procedures outside the OR
Pearl #9: Regional Nerve Blocks for Hip Fractures [14]
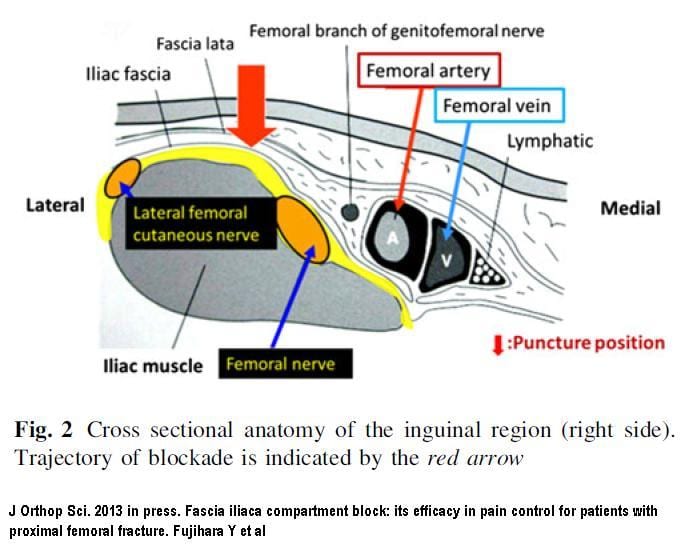
- What They Did: Multicenter RCT of 161 geriatric patients with hip fractures with US Guided Single Injection Femoral Nerve Block and then randomized to:
- Fascia Iliaca Block (FIB) by Anesthesiology within 24 hours
- Conventional Analgesics
- Fascia Iliaca Block Superior to Conventional Analgesics
- Improved Pain Control at 2 Hours
- Pain Scores at Rest, With Transfers out of Bed, and With Walking on POD 3 Improved
- At 6 Weeks Improved Walking and Stair Climbing Ability
- Required 33 – 40% Fewer Parenteral Morphine Sulfate Equivalents
- Study Bottom Line: Femoral nerve blocks result in superior outcomes in geriatric patients with hip fractures compared to parenteral pain medications
Pearl #10: Some Fun with Number Needed to Treat
- ASA in STEMI:
- NNT for Mortality = 42
- NNH for Minor Bleeding = 167
- NIPPV for COPD Exacerbation:
- NNT for Mortality = 8
- NNT for Avoiding Intubation = 5
- Abx for COPD Exacerbation:
- NNT for Mortality = 8
- NNT for Preventing Tx Failure = 3
- NIPPV for Acute Pulmonary Edema
- NNT for Mortality = 13
- NNT for Preventing Intubation = 8
- Heparin for ACS
- NNT to Prevent Nonfatal Heart Attack = 33
- NNH for Major Bleeding = 25
References:
- Willems JL et al. The Diagnostic Performance of Computer Programs for the Interpretation of Electrocardiograms. NEJM 1991. PMID: 1834940
- Durfey N et al. Severe Hyperkalemia: Can the Electrocardiogram Risk Stratify for Short-term adverse Events? West J Emerg Med 2017. PMID: 28874951
- Pasley J et al. Intraosseous Infusion Rates Under High Pressure: A Cadaveric Comparison of Anatomic Sites. J Trauma Acute Care Surg 2015. PMID: 25757113
- Moayedi S et al. Safety and Efficacy of the “Easy Internal Jugular (IJ)”: An Approach to Difficult Intravenous Access. JEM 2016. PMID: 27658558
- Peacock WF et al. Morphine and Outcomes in Acute Decompensated Heart Failure: An ADHERE Analysis. Emerg Med J 2008. PMID: 18356349
- Ikram et al. Haemodynamic and Hormone Responses to Acute and Chronic Furosemide Therapy in congestive Heart Failure. Clin Sci 1980. PMID: 7002435
- Wilson SS et al. Use of Nitroglycerin by Bolus Prevents Intensive Care Unit Admission in Patients with Acute Hypertensive Heart Failure. Am J Emerg Med 2017. PMID: 27825693
- Chaudry SI et al. Patterns of Weight Change Preceding Hospitalization for Heart Failure. Circulation 2007. PMID: 17846286
- Khandelwal N et al. Head-Eleavted Patient Positioning Decreases Complications of Emergent Tracheal Intubation in the Ward and Intensive Care Unit. Anesth Analg 2016. PMID: 26866753
- Driver BE et al. Flush Rate Oxygen for Emergency Airway Preoxygenation. Ann Emerg Med 2017. PMID: 27522310
- Caputo N et al. EmergeNcy Department use of Apneic Oxygenation Versus Usual Care During Rapid Sequence Intubation: A Randomized Controlled Trial (The ENDAO Trial). Acad Emerg Med 2017. PMID: 28791755
- Drew T et al. “The Invisible Gorilla Strikes Again: Sustained Inattentional Blindness in Expert Observers.” Psychol Sci 2014. PMCID: PMC3964612
- Beach ML et al. Major Adverse Events and Relationship to Nil per Os Status in Pediatric Sedation/Anesthesia Ouside the Operating Room: A Report of the Pediatric Sedation Consortium. Anesthesiology 2016. PMID: 26551974
- Morrison RS et al. Regional Nerve Blocks Improve Pain and Functional Outcomes in Hip Fracture: A Randomized Controlled Trial. J Am Geriatr Soc 2016. PMID: 27787895
Post Peer Reviewed By: Anand Swaminathan (Twitter: @EMSwami)
The post Clinical Pearls from ACEP 2017 – Washington D.C. appeared first on REBEL EM - Emergency Medicine Blog.
