
 Needs Assessment: As the COVID19 pandemic continues to mount, hospitals will rapidly reach maximal capacity. As a result, patients are boarding longer in the ED and, new patients are waiting longer to be seen. This dynamic poses numerous threats to patients safety. While we are seeing a large number of patients with severe and critical COVID19 who require intense monitoring, therapy and even ICU resources, many patients are only in need of supplemental O2 while they deal with their symptoms. The ability to discharge patients home with O2 and proper follow up monitoring can help open up more beds in both the ED and the hospital in general allowing us to deliver the proper resources to patients who need them.
Needs Assessment: As the COVID19 pandemic continues to mount, hospitals will rapidly reach maximal capacity. As a result, patients are boarding longer in the ED and, new patients are waiting longer to be seen. This dynamic poses numerous threats to patients safety. While we are seeing a large number of patients with severe and critical COVID19 who require intense monitoring, therapy and even ICU resources, many patients are only in need of supplemental O2 while they deal with their symptoms. The ability to discharge patients home with O2 and proper follow up monitoring can help open up more beds in both the ED and the hospital in general allowing us to deliver the proper resources to patients who need them.
Device Assignment Criteria
- Exertional O2 sat > 95% on RA – No device. Patient given follow up instructions
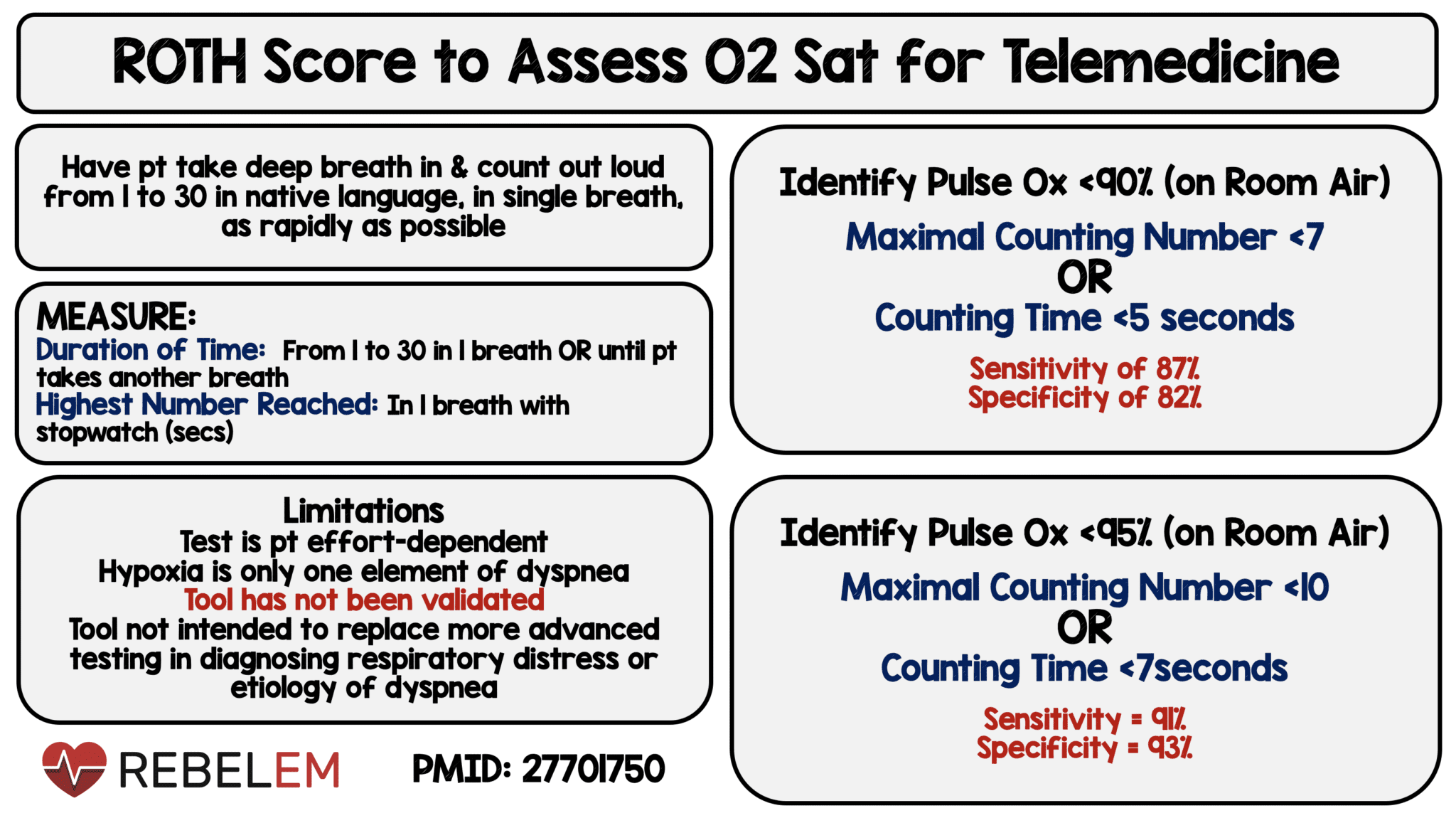
- Exertional O2 sat 92 – 95% on RA – Pulse Oximeter or Roth Score assessment by telemedicine in 24 hours
- Exertional O2 sat < 92: Enter into below protocol
Discharge Criteria
-
Disease Factors
- O2 saturation > 90% w/ < 5L via NC
- Walk test: Patient can walk 50 ft w/ O2 on w/o O2 sat < 90%
- Stable saturation on < 5 L NC in ED for 4 hours
- Patient Factors
- Age < 65
- Non-smoker going back to non-smoking household
- Returning to safe private residence and has a working phone number (Stable address and phone number which excludes homeless, shelter or temporary housed patients)
- Language restriction: English or Spanish speaking or has English speaking family member available for follow up appointments
- Clinical decision instrument (see below)
Clinical Decision Instrument Proposed Cutoffs
PORT/PSI:
- Moderate risk or lower (< 130 points)[Link is HERE]
MuLBSTA
- Will need to use a cutoff based on your comfort
- Department endorses a cutoff of < 15% mortality at 90 days [Link is HERE]
NB: Important to remember that while mortality or morbidity numbers may be high, there’s no evidence that hospitalization reduces this risk.
Necessary Supplies
- Oxygen Tank or Compressor (and ability to deliver additional tanks)
- Nasal Canula
- Oxygen Saturation Monitor (ideal)
Follow Up
-
Telemedicine appointment with Provider
- First call within 12-16 hours of discharge
- Subsequent calls Q24 X 3 days. If stable, move to Q3 days until symptom resolution
- Must have first appointment booked prior to discharge
- Must have video capability (i.e. Facetime, Skype, Zoom etc)
-
Telemedicine evaluation
- Each call should include expectant management (i.e. Come to hospital now, return for increasing symptoms, etc.)
- If patient has a primary care physician, consider a warm handoff to that physician after the first 2 follow up calls
- Discuss symptoms: should return for worsening shortness of breath or dyspnea or decreased exercise tolerance
- Check O2 tank: if running low, will have to arrange replacement
- Check Oxygenation (see below)
-
Return to hospital criteria
- Worsening shortness of breath or dyspnea
- Decreased exercise tolerance
- RR > 30 with exertion
- O2 Sat Monitor: sat < 90% on 5L NC
-
No O2 Sat Monitor: Roth Score (see below)
- Max counting number < 7 OR
- Counting time < 5 seconds
- NB: we recognize that the ROTH score is suboptimal but, we need an option in low resource settings where pulse oximeters are not available for patients to go home with
References:
- Chorin E et al. Assessment of Respiratory Distress by the Roth Score. Clin Card 2016; 39(11): 636-9. PMID: 27701750
Post Peer Reviewed By: Salim R. Rezaie, MD (Twitter: @srrezaie)
The post COVID-19: Home O2 Protocol appeared first on REBEL EM - Emergency Medicine Blog.
