
 The protected code blue is designed to keep your staff safe when managing a patient with COVID-19 who has a sudden cardiac arrest. You will continue to do high quality CPR, defibrillation (if indicated), give code medications, and BVM with airway management, now with a drape. I’m going to outline a suggested plan for how to conduct a protected code blue at your hospital. You will need to modify it to fit your hospitals requirements.
The protected code blue is designed to keep your staff safe when managing a patient with COVID-19 who has a sudden cardiac arrest. You will continue to do high quality CPR, defibrillation (if indicated), give code medications, and BVM with airway management, now with a drape. I’m going to outline a suggested plan for how to conduct a protected code blue at your hospital. You will need to modify it to fit your hospitals requirements.
Outline:
- Limit personnel in the room and clearly define roles
- Proper Personal Protective Equipment (PPE)
- The process of protected code blue
Personnel
Decide on the number of team members you need ahead of time. I suggest you need 4 people in the room to run the code. You should have 1 or 2 team members outside the room in PPE ready to enter if the team needs help or extra equipment is needed.
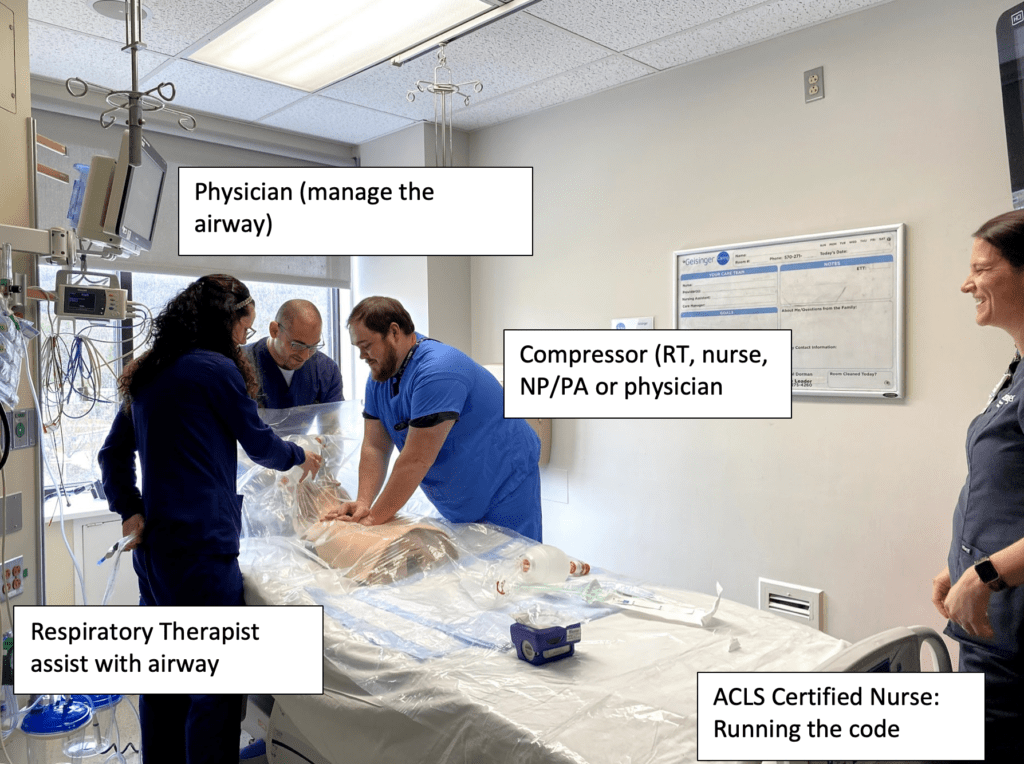
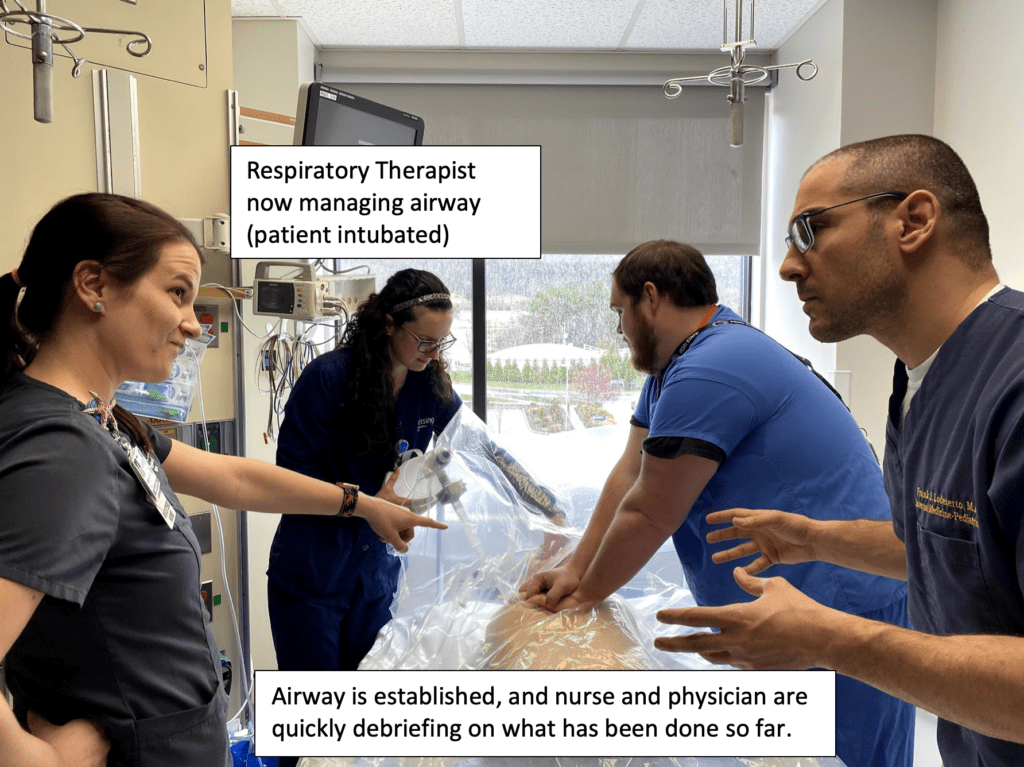
During the code, the most experienced airway operator (EM, CCM, Anesthesia) should be at the head of the bed managing the airway. You can decide to intubate with a glidescope or use a supraglottic device such as King airway or LMA. I don’t suggest continued BVM as it will be tiresome to maintain a tight seal, and potentially would be more aerosolizing given difficulty of maintaining a good seal. Placement of either an endotracheal tube or a supraglottic device will free up the physician to assist the nurse in running the code, continue to think of other reversible causes, and be an extra compressor.
Proper Personnel Protected Equipment (PPE)
Treat the code as you would an aerosolizing procedure so team members should be in an N-95 mask, with goggles, face shield and hair cap or PAPR. Double gown with water resistant gown and double glove. Members should not enter the room until proper PPE donned.
The Process of Protected Code Blue
The first team member entering the room in full PPE and should place a premade durable, clear drape over the patient. We have these available on our code carts. Our dimensions are 50 inches x 100 iches, however you can cut these to meet your hospitals needs.
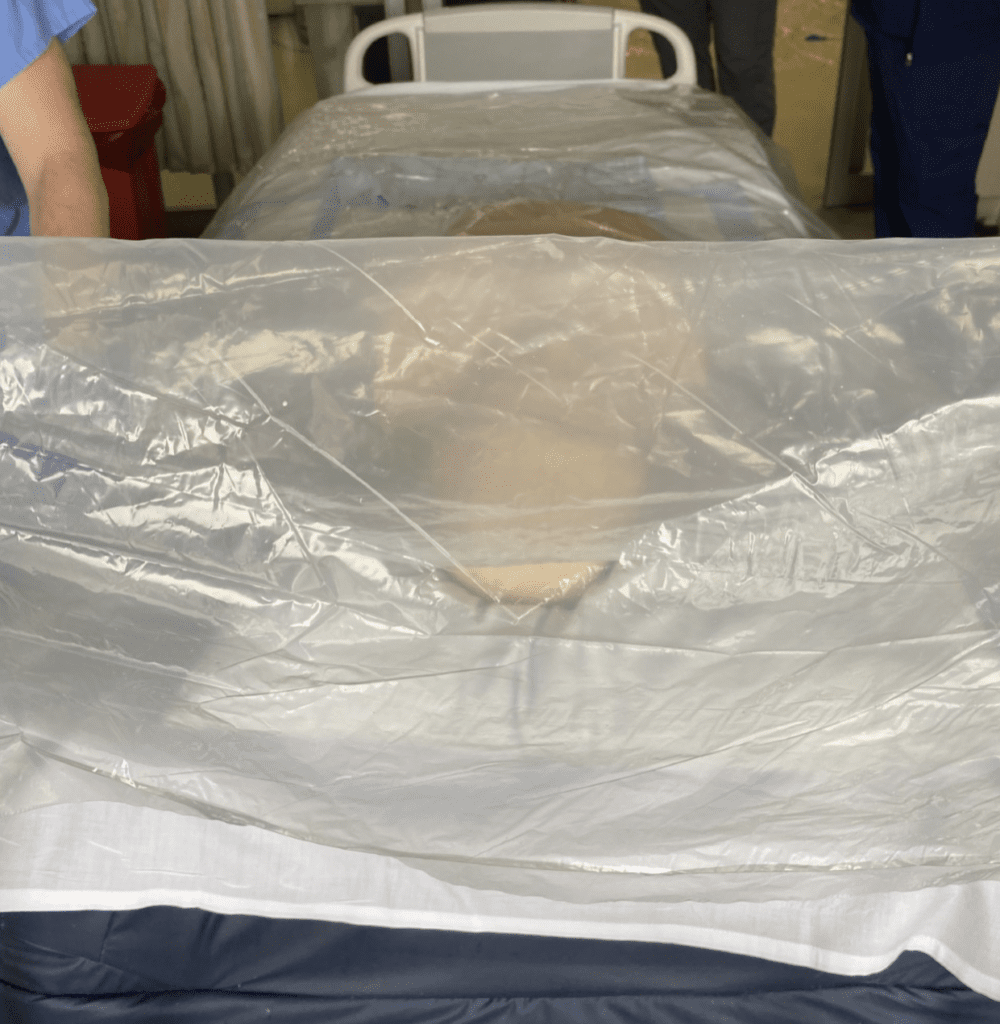
CPR can be performed easily over the clear drape, and defibrillator pads can be placed on the patient under the drape. A mechanical chest compressor may also be used under your drape based on your hospitals code blue procedure.
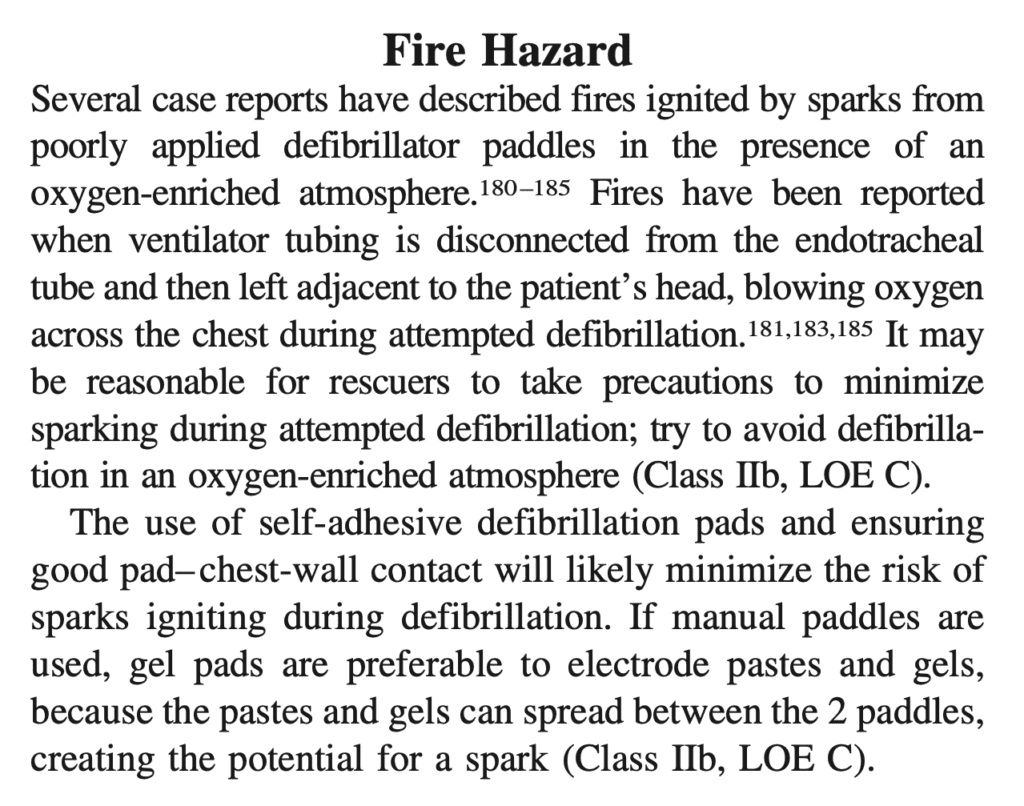
From the 2010 AHA Guidelines [2]
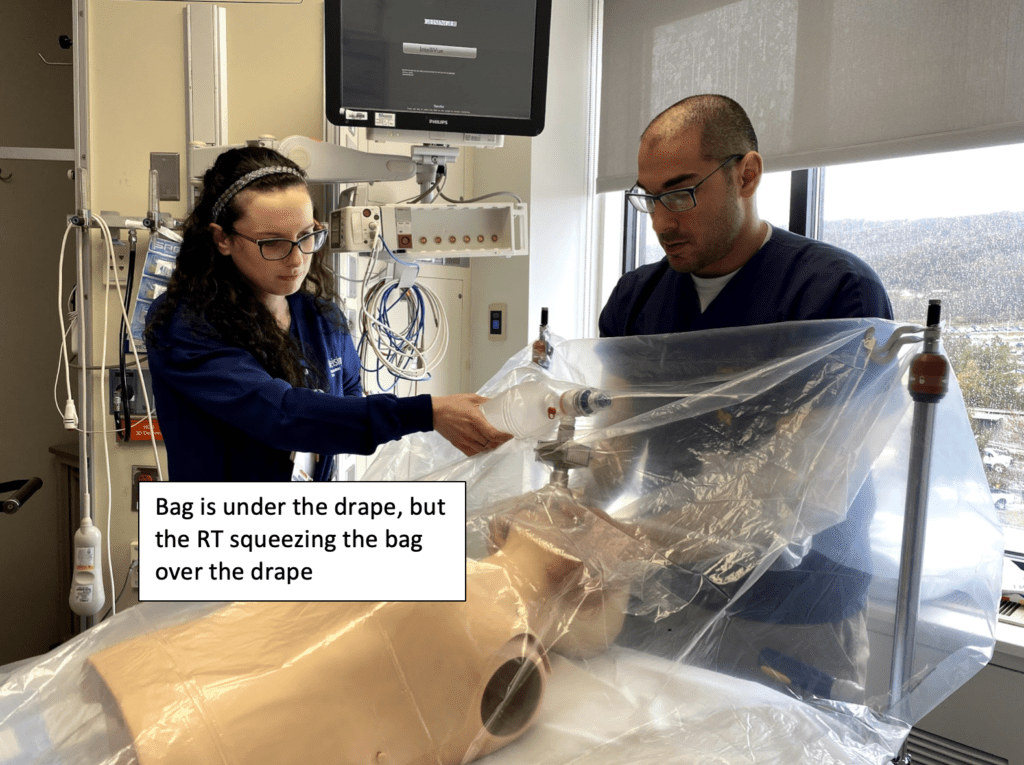
Airway management can happen under the drape. We suggest 2 team members performing BVM. We suggest a respiratory therapist delivering breath either under the drape or squeezing the bag outside the drape with the bag under the drape.
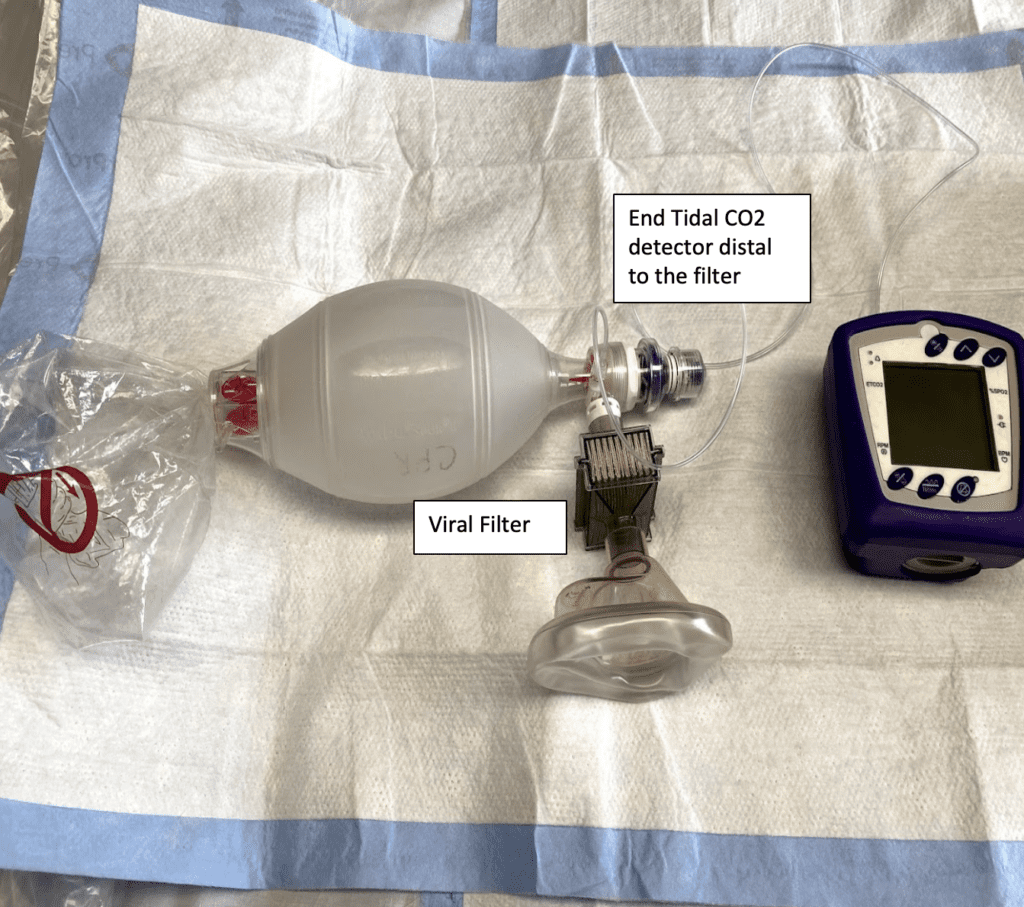
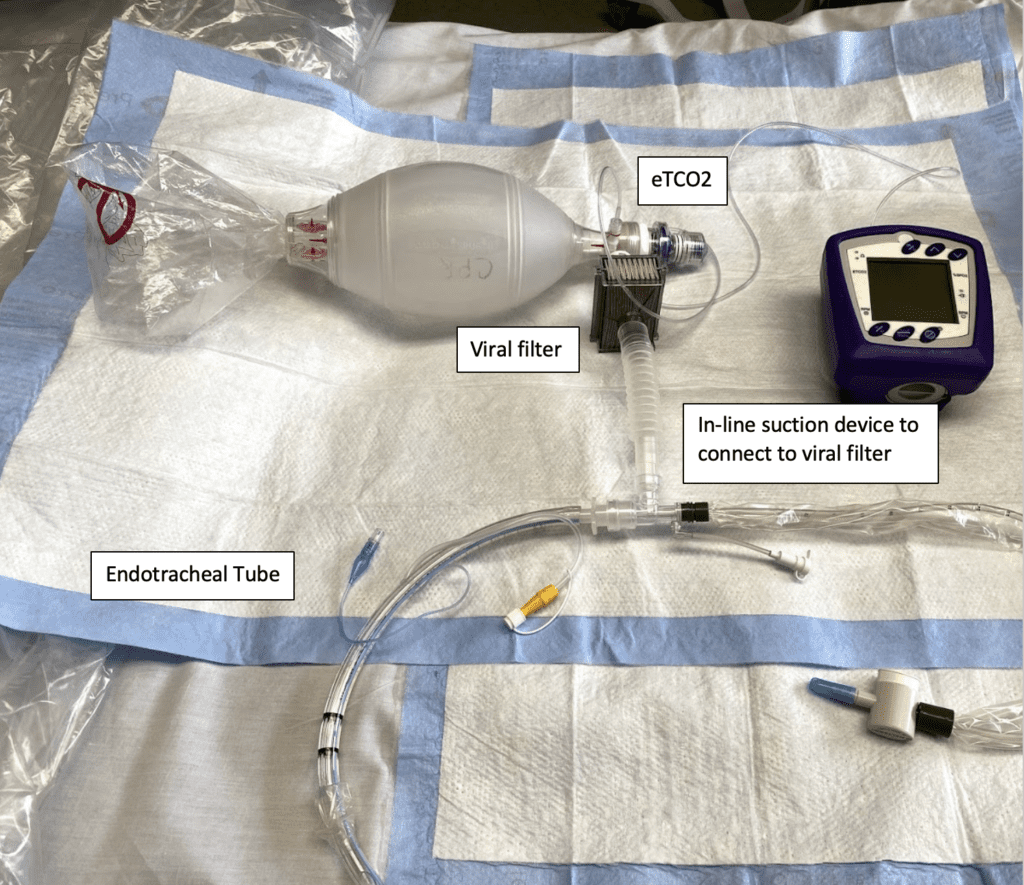
For BVM we suggest a viral filter between the mask and the bag.
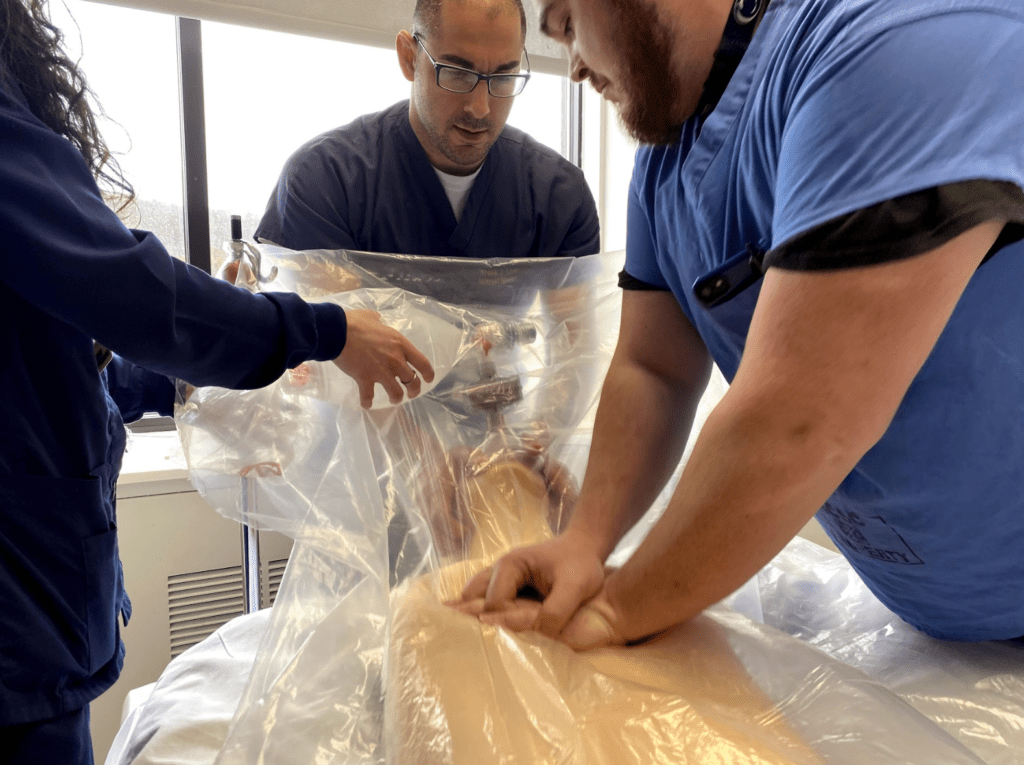
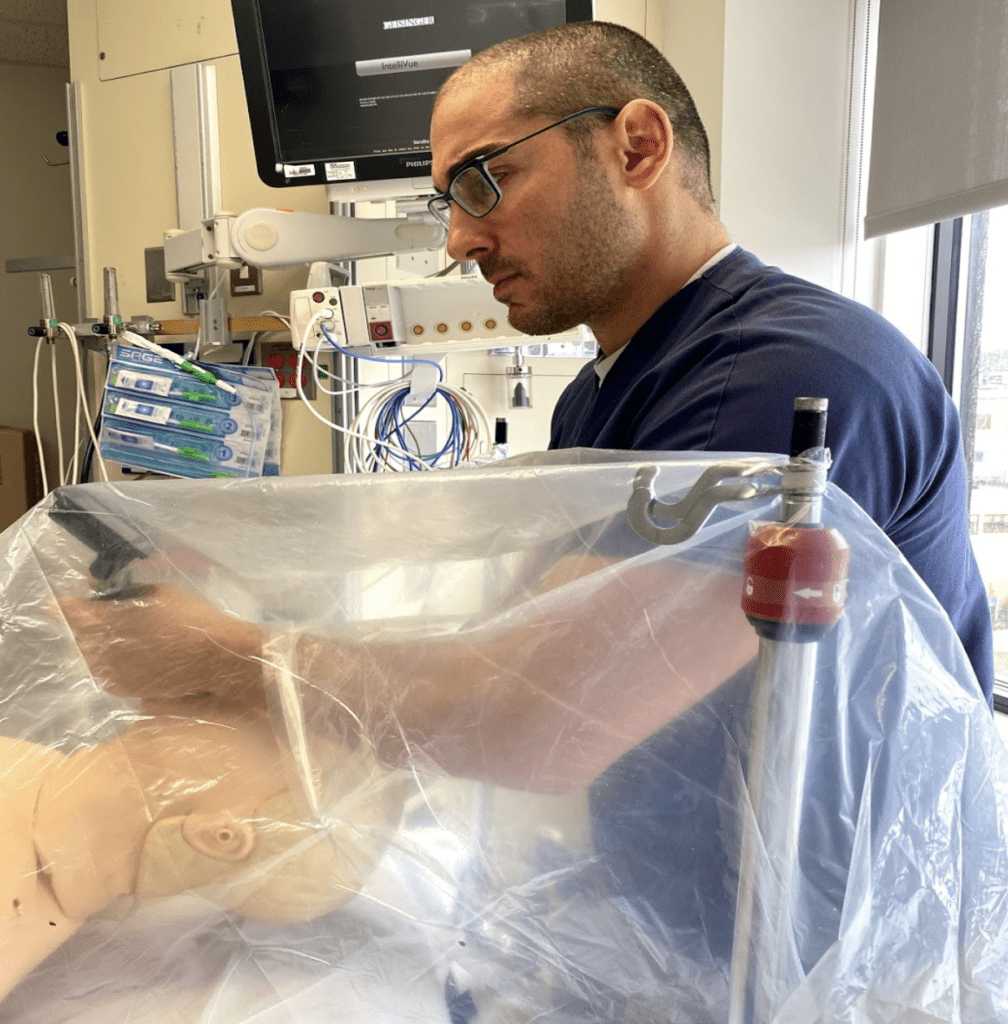
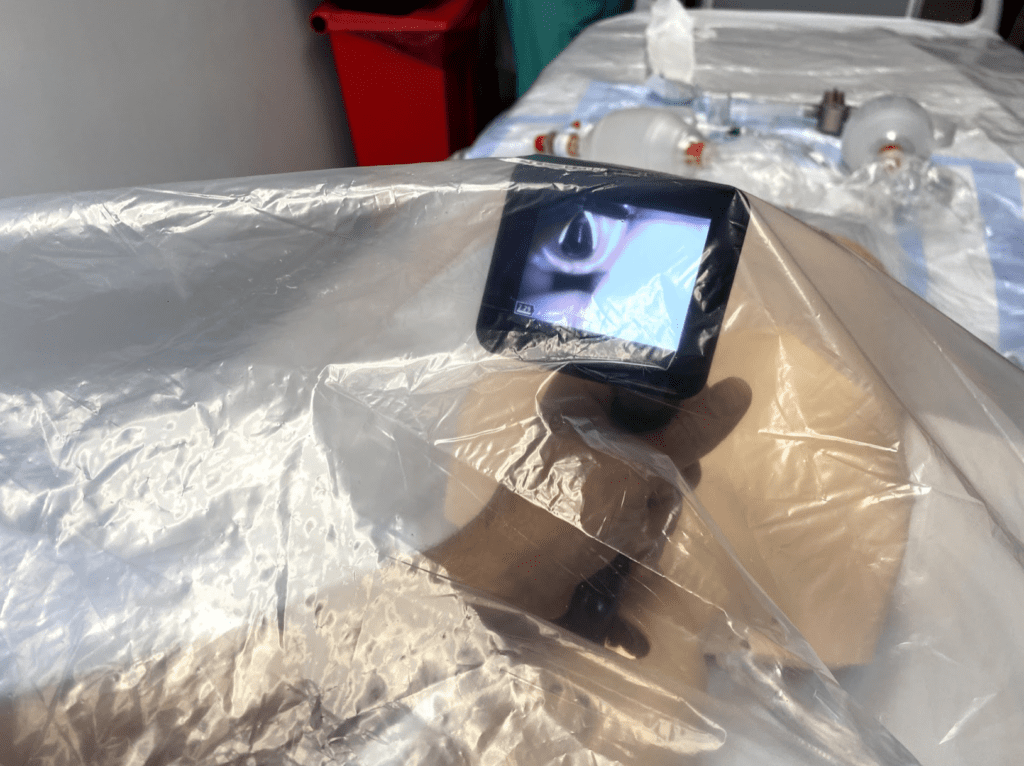
You can intubate under the drape as the drape is clear. Here we are using a portable glidescope device under the drape with an excellent view of the screen. You can also use a standard glidescope, with the screen outside of the drape, but still keeping your hands under the drape.
Note: This protected protocol of using the drape can be used for intubations as well as extubations, not just in the setting of a code blue.
Once the endotracheal tube is in place, ensure the cuff is inflated. Before connecting the bag directly to the endotracheal tube connect your viral filter and end tidal CO2 detector distal to the filter. Some viral filters do not directly connect to your endotracheal tube, so you may have to place a connector first. In our example, our filters don’t fit directly onto our endotracheal tubes, so we are using an in-line suction catheter tubing to serve as an adaptor to fit the viral filter. Another feasible option would be to connect to the ventilator instead of the BVM to remove an additional step and minimize potential aerosolization.
Code Discussions:
The purpose of the protected code blue is to deliver high quality CPR and keep your staff safe during this process. All patients, but in particular patients with moderate to severe symptoms related to COVID-19, need to have their code status addressed as early as possible. Not to get into an ethical debate, but older patients (>65 years old), with ARDS and multi-organ failure have high mortality rates1. These patients may or may not already be intubated. The chance of survival in these patients is low and an honest discussion with the patient or their family is essential. The utility of coding a patient with ARDS and multi-organ failure is beyond the scope of this post, but merely to start the discussion with your institution’s key stakeholders such as emergency medicine, critical care medicine, hospitalists services and palliative care. In my mind the purpose of running this code would to manage patients that have now become hypoxemic after failing conventional therapy such as NIV or high flow nasal cannula. Another reason may be also to treat reversible causes quickly such as a tension pneumothorax, mucous plugging or dysthymia’s related to possible underlying cardiomyopathy to name a few.
Special Thanks To:
Danielle Butler RN
Tara Little RT-ACCS
Joshua Vanhouten RT-ACCS
Mark Reffner RT-ACCS
Angela Bower RN
References:
- Yang et al. Clinical Course and Outcomes of Critically ill Patients with SARS-CoV-2 Pneumonia in Wuhan, China: A Single-Centered, Retrospective, Observational Study. Lancet 2020. PMID: 32105632
- Link MS et al. Part 6: Electrical Therapies: Automated External Defibrillators, Defibrillation, Cardioversion, and Pacing: 2010 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation 2010. PMID: 20956222
For More Thoughts on This Topic Checkout:
- EMCases: COVID-19 – Protected Intubation
- ERCast: COVID-19 – Protected Code Blue
- AliEM: Trick of the Trade – Identifying Team Members in Protected Code Blues
Post Peer Reviewed By: Salim R. Rezaie, MD (Twitter: @srrezaie)
The post COVID-19: Protected Code Blue appeared first on REBEL EM - Emergency Medicine Blog.
