
 While the rate of prepublications on COVID19 continue to be cranked out, we at REBEL EM have reduced our blog post production. It’s not because we’re reading less, but we’ve reported enough on small, retrospective, observational studies that don’t tell us anything more than we already know. At this point in time we know enough about what does and doesn’t work, so we wanted to focus on important literature that may affect practice. Going forward that will be our focus with updates in a less rapid-fire rate and more useful way to digest the information. For this COVID-19 update we have picked four papers that are we thought are worthy of mention.
While the rate of prepublications on COVID19 continue to be cranked out, we at REBEL EM have reduced our blog post production. It’s not because we’re reading less, but we’ve reported enough on small, retrospective, observational studies that don’t tell us anything more than we already know. At this point in time we know enough about what does and doesn’t work, so we wanted to focus on important literature that may affect practice. Going forward that will be our focus with updates in a less rapid-fire rate and more useful way to digest the information. For this COVID-19 update we have picked four papers that are we thought are worthy of mention.
The Aerosol Box is Potentially Dangerous [1]
Begley JL et al. The Aerosol Box for Intubation in COVID-19 Patients: An In-Situ Simulation Crossover Study. Anaesthesia 2020. [Epub Ahead of Print]
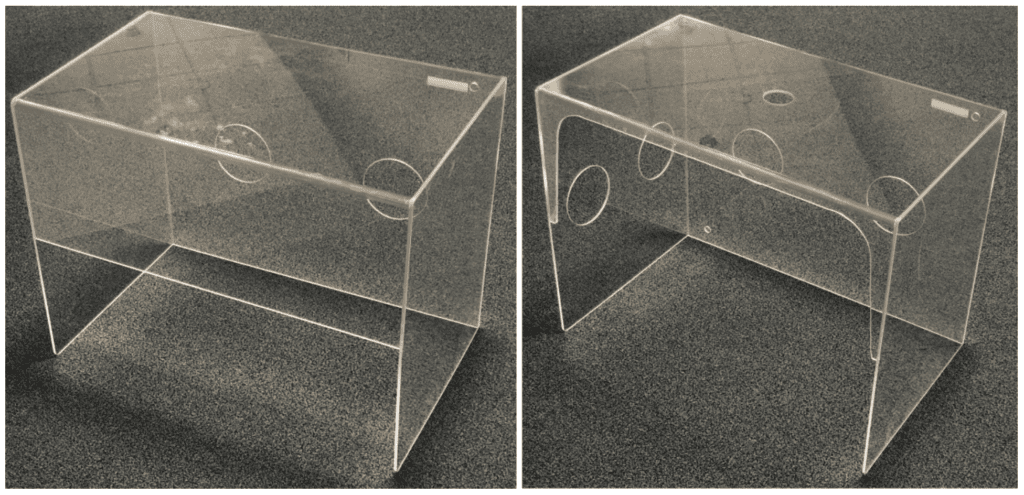
In our efforts to meet the dual challenge of caring for highly infectious patients and protecting ourselves, we’ve seen the use of novel, untested, unproven devices seep into the clinical environment. One such device is theaerosol box; a transparent plastic cube covering a patient’s head and shoulders with access holes for intubating. Some models add additional holes for an assistant to access the patients head and face as well (see figures below).
This article discussed two important biases that were new to me:
- Gizmo Idolatry: Implicit conviction that a more technological approach is intrinsically better than one that is less technological
- MacGyver bias: Inherent attraction of our own personal improvised devices
This was an in-situ simulation crossover study looking at the impact of two aerosol boxes on intubations of a simulated patient with severe COVID-19 in the ICU. 12 consultant anesthesiologists, with extensive airway experience performed 3 intubations each (no aerosol box, and one with each of the aerosol boxes), totaling 36 intubations. Anesthetists wore PPE consistent with local guidelines for intubation of a patient with COVID-19, consisting of a face-shield, goggles/glasses, mask, gown and gloves (Due to concerns about PPE stocks, a surgical mask was worn instead of a P2/95 mask and standard clinical gloves instead of long-cuffed surgical gloves). All anesthetists elected to use a bougie 1st approach with video laryngoscopy as their standard approach.
The primary outcome was intubation time (defined as the time from removing the facemask until the 1st breath was delivered by a correctly placed endotracheal tube with an inflated cuff). Secondary outcomes included 1stpass intubation success, intubation grade (modified Cormack-Lehane grade, on the video screen, breaks in pre-oxygenation mask-seal, and breaches/damage to PPE.
Critical Results:

Of the 8 breaches in PPE, one tear was in the gown sleeve and the remainder were gowns pulled back from the glove exposing the skin. All breaches appeared to be due to the gown becoming stuck or held-up at the arm hole or the occlusive dressings used on the arm holes. None of these breaches represents a high-risk SARS-CoV exposure.
The most frequently mentioned factors relating to the aerosol boxes were:
- Discomfort of arms/back/knees: 50%
- Increased cognitive load: 33%
Bottom Line: The observed delays in intubation are clinically important, as the desaturation of patients with COVID-19 on induction can be rapid and profound. Safety for both patient and staff is of utmost importance (efficient intubation to avoid patient harm from hypoxia as well as the device not compromising PPE) when deciding when to use a novel device. Although the sample size was small, and the methodology was in a simulation setting, the clinical impacts are important: Aerosol boxes prolong intubation times while leading to potential PPE compromise. Additionally it is unclear if aerosol boxes offer any increased protection from infectious droplets or airborne contaminants.
Awake Proning to Improve Patient Oriented Outcomes? Maybe…[2]
Elharrar X et al. Use of Prone Positioning in Nonintubated Patients With COVID-19 and Hypoxemic Acute Respiratory Failure. JAMA 2020. [Epub Ahead of Print]
This was a small, prospective, single-center, before-after study conducted on awake nonintubated, COVID19 patients with hypoxemic acute respiratory failure requiring oxygen supplementation performed in France. To be eligible patients had to meet two criteria: 1. Required O2 supplementation and 2. Had chest CT findings suggestive of COVID-19 with posterior lesions. Arterial blood gases were drawn just before proning, during proning and 6 to 12 hours after resupination.
Important definitions:
- During prone positioning = 1 to 2 hours after patients were placed in prone position
- After resupination = 6 to 12 hours after resupination
- Responder to prone positioning = Increased PaO2 ≥ 20% after prone positioning
- Persistent responder to prone positioning = PaO2 increase ≥20% after resupination (in comparison to before proning)
The main outcome was the proportion of responders. There were a number of secondary outcomes including feasibility (proportion of patients sustaining prone positioning ≥1hr and ≥3hrs). Patients were followed up to 10 days.
25 patients were eligible for assessment, and 24 agreed to participate. 67% of patients were on <4LPM nasal oxygen and 33% were on ≥4LPM or HFNC (No NIV). It is unclear what prone positioning exactly means in this study. I am going to assume this is full prone positioning and not frequent repositioning which may be better tolerated.
Critical Findings:
- Responder to Prone Positioning: 6/24pts (25%)
- Responder to Prone Positioning + Sustained Prone Positioning ≥3hrs: 6/15pts (40%)
- Persistent Responders of Prone Positioning = 3/24pts (12.5%)
- Mean PaO2 Increase in Sustained Prone Positioning ≥3hrs:
- Before Prone Positioning: 73.6mmHg
- During Prone Positioning: 94.9mmHg
- No difference between PaO2 before prone positioning and after resupination
Able to Tolerate Prone Positioning (No sedation or anxiolytics were used):
- <1hr: 4pts (17%)
- 1 to 3hrs: 5pts (21%)
- ≥3hrs: 15pts (63%)
No patients experienced major complications, but 10/24pts (42%) reported back pain during proning
At the end of a 10d follow-up period, 5 patients required invasive mechanical ventilation (4/5 did not sustain prone positioning for ≥1hr)
Bottom Line: In patients who tolerated prone positioning, oxygenation increased in 25% of patients, but was not sustained in half of those after resupination. While the prone position can improve oxygenation and potentially result in less injurious ventilation, this does not necessarily equate to lung protection and better outcomes. We still need a larger trial to show that improved oxygenation during prone positioning (surrogate outcome) improves mortality (patient oriented outcome). Two things are clear from this study:
- Duration of proning is important in this disease: You are not gonna reverse pathology with a couple of hours of proning as the disease process takes much longer to improve based on prior experiences
- If doing awake prone positioning, frequent assessment of work of breathing is essential to avoid delayed intubation, which has certainly been shown to worsen mortality (For more specifics on reassessment look at Swami’s post on Awake Proning –> Link is HERE).
COVID-GRAM: A Clinical Prediction Rule to Predict Critical Illness in Hospitalized COVID-19 Patients [3]
Liang W et al. Development and Validation of a Clnical Risk Score to Predict the Occurrence of Critical Illness in Hospitalized Patients with COVID-19. JAMA Intern Med 2020. PMID: 32396163
This was a retrospective cohort study looking to derive and validate a clinical risk score that could predict which admitted COVID19 patients are likely to develop critical illness (Defined as a composite of admission to ICU, mechanical ventilation, or death).
For the derivation cohort, 1590 patients from 575 hospitals in China were included. 72 variables were evaluated in the selection process. Logistic regression models were used to show statistically significant factors which were then used to construct the COVID-GRAM risk score (Found online in Chinese and English – Link is HERE) to predict the likelihood of critical illness. The accuracy of the risk score was assessed using the area under the receiver-operator characteristic curve (AUC). The validation cohort included 710 patients from 3 hospitals plus amassed data from hospitals in 20 other cities not included in the derivation cohort were used.
Results:
- In the derivation cohort, 1.5% of patients had severe disease on presentation with an additional 131 patients (8.2%) developing critical illness. The overall mortality in this group was 3.2%.
- Of the 72 potential variables, 10 of them were independently statistically significant predictors of critical illness and included in the risk score:
- CXR abnormality (OR 3.39; 95% CI 2.14 to 5.38)
- Age (OR 1.03; 95% CI 1.01 to 1.05)
- Hemoptysis (OR 4.53; 95% CI 1.36 to 15.15)
- Dyspnea (OR 1.88; 95% CI 1.18 to 3.01)
- Unconsciousness (OR 4.71; 95% CI 1.39 to 15.98)
- Number of Comorbidities (OR 1.60; 95% CI1.27 to 2.00)
- Cancer History (OR 4.07; 95% CI 1.23 to 13.43)
- Neutrophil-to-Lymphocyte Ratio (OR 1.06; 95% CI 1.02 to 1.10)
- LDH (OR 1.002; 95% CI 1.001 to 1.004)
- Direct Bilirubin (OR 1.15; 95% CI 1.06 to 1.24)
- Accuracy of COVID-GRAM to predict likelihood of critical illness in the derivation cohort was AUC 0.88 (95% CI 0.85 to 0.91)
- This score performed better than CURB-65 (AUC 0.75; 9% CI 0.70 to 0.80) in the prediction of critical illness
- In the validation cohort, critical illness eventually developed in 87 patients (12.3%) and of these patients 8 (1.1%) died
- The accuracy of the COVID-GRAM risk score to predict likelihood of critical illness was similar to the validation cohort (AUC 0.88; 95% CI 0.84 to 0.93)
Discussion:
- Several factors that have been shown in other studies as predictors of severity of disease were evaluated but not found to be statistically significant (i.e. D-dimer and CRP, etc…)
Limitations:
- Dyspnea is not well defined in this trial. For example, is this a RR of >30, work of breathing, or some combination of both?
- This score was based on a health system and patient population based solely out of China. This would need to be validated before implementation
- Part of severity of illness was admission to ICU, but this is a subjectively decided parameter, which sill differ from physician to physician and institution to institution
- 575 hospitals contributed data for the derivation cohort of 1600 patients. This most likely means lots of patients were missed from these hospitals (i.e. unlikely hospitals averaged <3patients/hospital)
- Retrospective derivation with retrospective validation. Would need both prospective and external validation
- This is not a simple score and cannot be calculated in our heads. Will need a calculator which might reduce extrapolation to clinical practice
- Being admitted to the ICU vs death are not equal outcomes and it is unclear from this study or this score which thing we are actually predicting
Bottom Line: Earlier prediction of critical illness in hospitalized patients with COVID-19 could support more aggressive treatment (see next paper) or pre-emptive admission to the ICU. COVID-GRAM is the first clinical prediction score, and I am sure not the last, to assess the likelihood of development of critical illness in COVID-19 patients admitted to the hospital with good accuracy. However, the use of unequal composite outcomes, subjective nature of some variables, and lack of several factors shown in other literature to be significant predictors of critical illness (i.e. d-dimer), the exact utility of this score is not clinically clear.
Do the Basics Well [4]
Sun Q et al. Lower Mortality of COVID-19 by Early Recognition and Intervention: Experience from Jiangsu Province. Ann Intensive Care 2020. [Epub Ahead of Print]
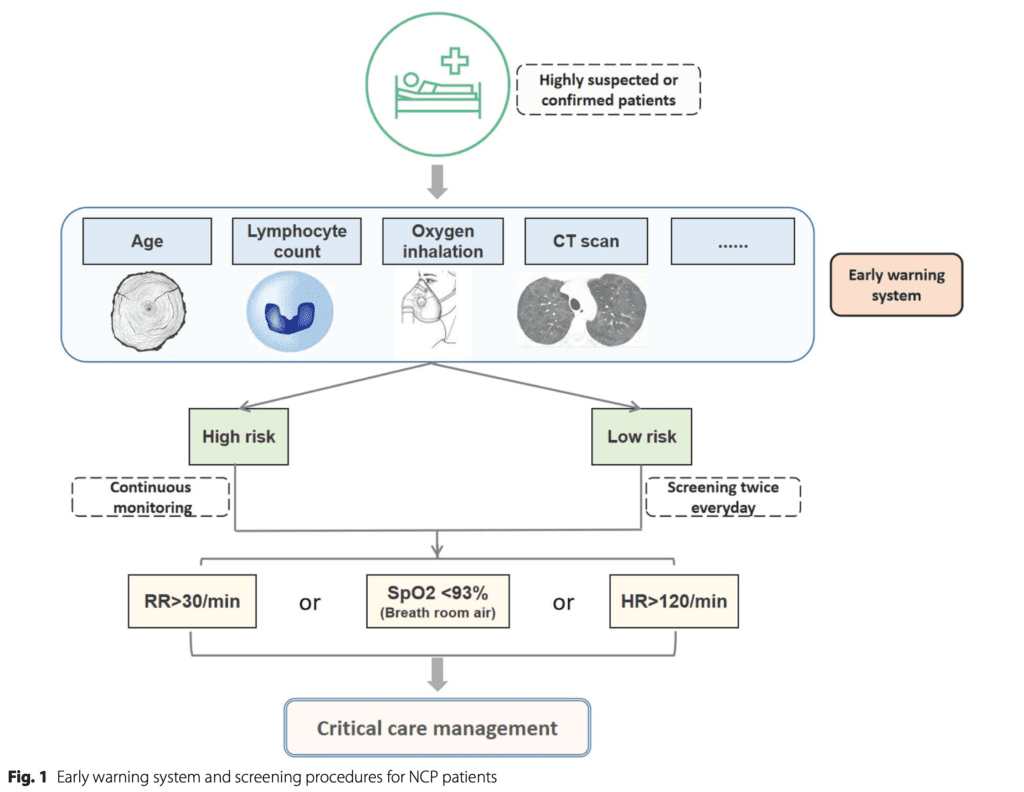
This is a letter to the editor about 631 patients with confirmed COVID-19 pneumonia with discharge from hospital and cure rate of 96.67%. In this letter to the editor the authors discuss their basic and essential strategies to improve outcomes highlighting early detection of high-risk and critically ill patients.
From their >600 patients with COVID-19 pneumonia the authors state age, lymphocyte count, oxygen supplementation, and aggressive pulmonary radiographic infiltrations were all independent risk factors for COVID-19 pneumonia progressing into a critical condition. The developed an early warning system combining these 4 factors. Although data is yet unpublished, the authors state the sensitivity of this system was 0.955 (95% CI 0.772 to 0.999), the specificity was 0.899 (95% CI 0.863 to 0.928) and the area under ROC curve was 0.962.
There focus was on three things (the basics) which have an evidence base in preventing tracheal intubation:
- For patients with ARDS or extensive pulmonary infiltrates: HFNC or NIV to maintain PEEP to prevent alveolar collapse (even in patients without hypoxemia)
- Restrictive fluid resuscitation to relieve pulmonary edema
- Awake prone positioning which improved oxygenation and pulmonary heterogeneity
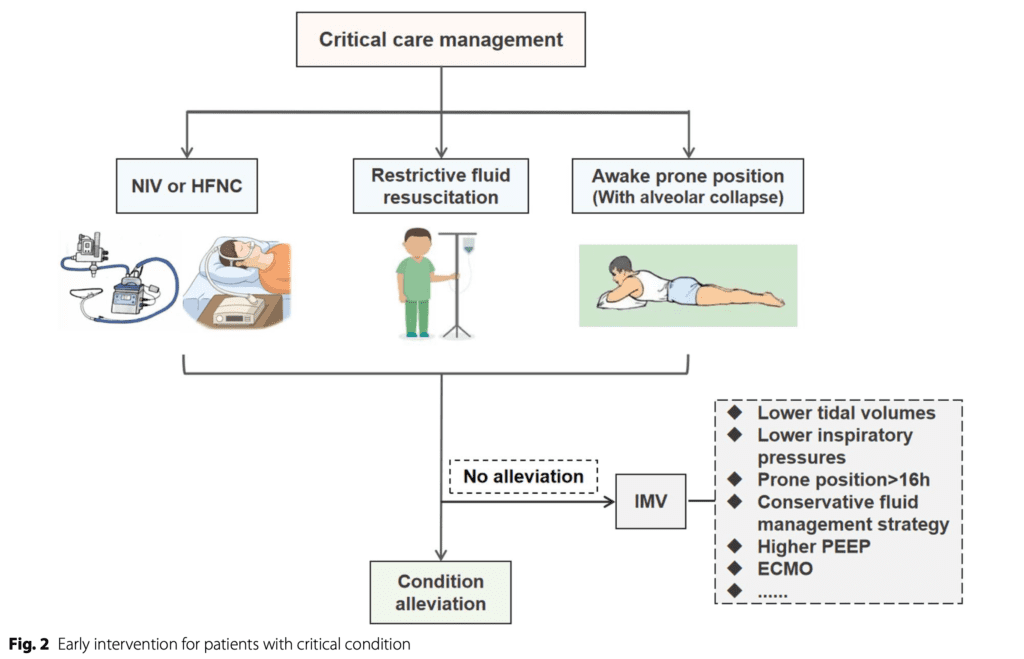
What did all this achieve?
- With a 10% critically ill patient population, the invasive mechanical ventilation rate was <1% (We don’t don’t how critically ill was defined nor what the overall denominator of patients was for this study)
- Another important point is the number of staff available: 234 clinical staff invested in COVID-19 pneumonia treatment and care, 3500 clinical staff reserved for unexpected needs. These are absolutely amazing numbers giving impressive clinician to patient ratios
Bottom Line: Do the basics well, which is simply just good patient care.
- Identify pts early (RR >30 OR SpO2<93% OR HR >120)
- Support O2 with HFNC and/or NIV
- Restrict fluids (but not too much)
- Awake proning or frequent position changing
- Evaluate pts frequently
References:
- Begley JL et al. The Aerosol Box for Intubation in COVID-19 Patients: An In-Situ Simulation Crossover Study. Anaesthesia 2020. [Epub Ahead of Print]
- Elharrar X et al. Use of Prone Positioning in Nonintubated Patients With COVID-19 and Hypoxemic Acute Respiratory Failure. JAMA 2020. [Epub Ahead of Print]
- Liang W et al. Development and Validation of a Clnical Risk Score to Predict the Occurrence of Critical Illness in Hospitalized Patients with COVID-19. JAMA Intern Med 2020. PMID: 32396163
- Sun Q et al. Lower Mortality of COVID-19 by Early Recognition and Intervention: Experience from Jiangsu Province. Ann Intensive Care 2020. [Epub Ahead of Print]
Post Peer Reviewed By: Anand Swaminathan, MD (Twitter: @EMSwami)
The post COVID-19 Update: Aerosol Box, Awake Proning, Prediction Scores, & Doing the Basics Right appeared first on REBEL EM - Emergency Medicine Blog.


