
 Background: Cricoid pressure is dead, right? Many have made this claim including a brilliant argument against its use by John Hinds here. Despite the many eulogies, we continue to hear about cricoid pressure so it makes sense that we dive in to the background prior to addressing the recent JAMA Surgery publication.
Background: Cricoid pressure is dead, right? Many have made this claim including a brilliant argument against its use by John Hinds here. Despite the many eulogies, we continue to hear about cricoid pressure so it makes sense that we dive in to the background prior to addressing the recent JAMA Surgery publication.
Cricoid pressure was first described by Dr. Sellick in the 1960’s though similar techniques were described as far back as the 1770s (Sellick 1961). The Sellick’s maneuver entailed the application of pressure over the cricoid cartilage with the thumb and 1-2 additional fingers. The goal was to compress the cricoid cartilage against the esophagus in order to occlude the esophagus and prevent regurgitation of stomach contents into the upper airway. Initial studies on the maneuver suffered from a bevy of methodological flaws including small n, lack of blinding or randomization and selection bias. Despite this, Sellick’s maneuver was widely adopted and taught to hordes of anesthesia, critical care and emergency residents.
Studies investigating cricoid pressure in the last decade have demonstrated a number of issues with claims that it can prevent passive regurgitation. Check out this free chapter on EMRAP for an in depth discussion. Dynamic MRI studies demonstrate that application of pressure to the cricoid cartilage displaces the esophagus laterally instead of occluding it (Smith 2003, Boet 2012). An ultrasound study demonstrated similar findings: in 60% of patients the esophagus was lateral to the airway and cricoid pressure led to displacement rather than occlusion in all patients. (Tsung 2012).
Additionally, application of cricoid pressure decreases airway patency and increases the chance that your view of the airway will be obscured. (Allman 1995, Palmer 2000, Smith 2002, Oh 2013). Finally, no study to date has demonstrated a reduction in aspiration episodes with the application of cricoid pressure. A large observational study of pregnant patients undergoing C-sections found no difference in aspiration events and that the overall aspiration event rate was low (Fenton 2009). However, up until this point, there has not been a high-quality, randomized controlled trial performed.
Article: Birenbaum A et al. Effect of cricoid pressure compared with a sham procedure in the rapid sequence induction of anesthesia: The IRIS Randomized Clinical Trial. JAMA Surgery 2018. PMID: 30347104
Clinical Question: Does the application of cricoid pressure prevent pulmonary aspiration in patients undergoing rapid sequence induction of anesthesia?
Population: Patients > 18 years of age undergoing general anesthesia in the operating room with < 6 hours of fasting time or the presence of at least 1 risk factor for pulmonary aspiration (emergency conditions, BMI > 30, previous gastric surgery, ileus, < 48 hours postpartum, diabetic gastroparesis, gastroesophageal reflux, hiatal hernia, preoperative nausea/vomiting and pain.
Outcomes:
- Primary: Incidence of pulmonary aspiration (either visually detected at the glottis during laryngoscopy or by tracheal aspiration just after tracheal intubation)
- Secondary: Frequency of suspected aspiration pneumonia within 24 hours, difficult tracheal intubation (Cormack + Lehane grade, cricoid pressure interruption, frequency of difficulty intubation, need to provide mask ventilation, O2 sat < 92%) and traumatic complications. Difficult intubation defined as requiring > 2 attempts or alternative technique used (except for gum elastic bougie)
Intervention: “Sham” cricoid pressure (hand under opaque cover applying no pressure)
Control: Sellick’s maneuver (30 N of face applied to the cricoid cartilage with 3 fingers (hand under opaque cover)
Design: Multicenter, randomized, double-blind, non-inferiority trial
Excluded: Patient refusal to participate, pregnancy, inclusion in another randomized trial, lack of national health care insurance, contraindication for the use of cricoid pressure or succinylcholine, pneumonia or pulmonary contusion, upper respiratory tract abnormalities, consciousness disorders and patients requiring an alternate technique to laryngoscopy.
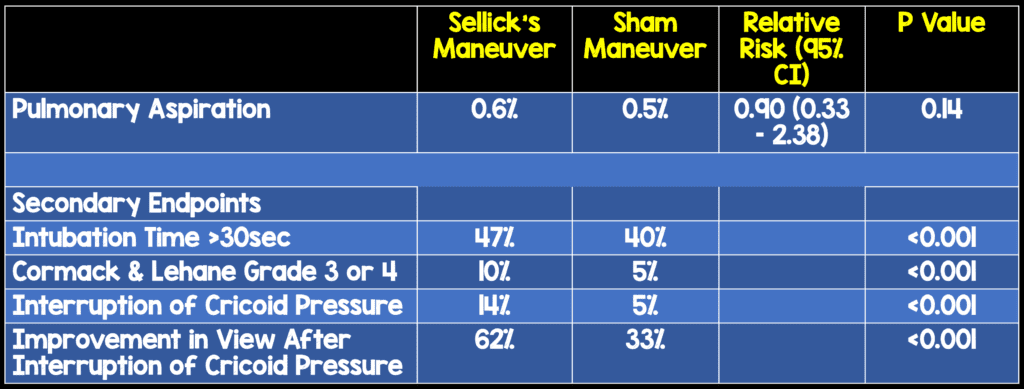
Primary Results:
- 10 centers participated in enrollment of patients
- 3472 patients were recruited with one patient withdrawing consent in the Sellick’s maneuver group
-
A priori Statistical Analysis
- Base pulmonary aspiration rate of 2.8% assumed
- Non-inferiority defined as an aspiration rate < 50% higher in the sham group (RR < 1.5)
- Required sample size based on these assumptions n = 3500
Critical Findings:
Strengths:
- This is the first large randomized trial investigating cricoid pressure
- Asks a clinically important, patient centered question
- Features many high-level study qualities – multicenter, randomization, blinding
- Baseline characteristics including level of training of operator were well balanced between groups
- Proper training was undertaken to ensure that those supplying cricoid pressure were performing it properly
- There were no major protocol violations and only 12 minor violations
Limitations:
- This is not a study of ED patients requiring emergency intubation so it is unclear exactly how to apply this to EM practice
- The randomization process is not explicitly discussed in the manuscript
- It is unclear how many patients were excluded from randomization
- Pregnant patients were excluded. This is important because aspiration is a significant cause of maternal death
- Pediatric patients were excluded. This evidence cannot be applied to this group
- Some patients had nasogastric tubes (13%) before anesthesia, and the decision to remove this was left up to the attending anesthesiologist as well as the decision to administer antacid (12%) before anesthesia, both of which could affect aspiration rates
- No standardization of patients with gastric tubes, although this did not change the results of this study
- The induction agent wasn’t standardized. It’s unclear if this would have affected the results, though.
- Power calculation based on a baseline pulmonary aspiration rate of 2.8% but the rate was considerably lower (just 0.6%) leading to wide confidence intervals around the point estimate
- Though the study was blinded, the intubator may have been aware of whether the patient was getting true cricoid pressure or the sham procedure. This may pose a limitation because pulmonary aspiration was gauged partly based on visualization of vomitus by the laryngoscope operator
Discussion:
- Technically, this is a negative study – it does not demonstrate non-inferiority of the “sham” maneuver in comparison to cricoid pressure. However, there is an absence of any hint of benefit to cricoid pressure from this data.
- The “sham” technique outperformed cricoid pressure in most secondary outcomes including quality of view, improvement of view with removal of criciod/“sham” pressure, intubation time and difficult intubations
Authors Conclusions:
“This large randomized clinical trial performed in patients undergoing anesthesia with RSI failed to demonstrate the noninferiority of the sham procedure in preventing pulmonary aspiration. Further studies are required in pregnant women and outside the operating room.”
Our Conclusions: Although this study failed to demonstrate non-inferiority of sham cricoid pressure to cricoid pressure the data does not show any hint that cricoid pressure is the better approach. In fact, there was a significant difference in terms of difficulty of intubation favoring no application of cricoid pressure and, the difficulty in view was relieved in most cases by removing cricoid pressure.
Potential to Impact Current Practice: Cricoid pressure should not routinely be provided to patients undergoing intubation.
Bottom Line: Occlusion of the esophagus by cricoid pressure appears to be a myth based on MRI and US studies. Previous literature demonstrates that cricoid pressure gives inferior views and no high-quality literature has shown decreased aspiration with application of cricoid pressure.
All of this in conjunction with the numbers seen in this study tells us that pulmonary aspiration is uncommon in the OR setting and isn’t reduced by the application of cricoid pressure. While an ED based study would be nice to have, the current evidence tells us that application of cricoid pressure is unlikely to benefit our patients but is likely to make our intubation more difficult.
“In our futile attempts to prevent this rarity [pulmonary aspiration] we actively thwart our own efforts in securing an airway.” – Rory Spiegel
For More on This Topic Checkout:
- EMCrit: Cricolol by John Hinds
- EMRAP: Medical Myths – Cricoid Pressure
- St. Emlyn’s: Cricoid Pressure and RSI, Do We Still Need It?
- EM Nerd: The Case of the Inferior Superiority
- First10EM: Cricoid Pressure is DEAD
References:
- Sellick BA. Cricoid pressure to control regurgitation of stomach contents during induction of anaesthesia. Lancet 1961; 404-6. PMID: 13749923
- Smith et al. Cricoid pressure displaces the esophagus: an observational study using magnetic resonance imaging. Anes 2003; 99(1): 60-4. PMID: 12826843
- Boet S et al. Cricoid pressure provides incomplete esopogeal occlusion associated with lateral deviation: a MRI study. J Emerg Med 2012; 42(5): 606-11. PMID: 21669510
- Tsung WJ et al. Dynamic anatomic relationship of the esophagus and trachea on sonography: Implications for endotracheal tube confirmation in children. J Ultrasound Med 2012; 31: 1365-70. PMID: 22922616
- Allman KG. The effect of cricoid pressure application on airway patency. J Clin Anes 1995; 7: 197-9. PMID: 7669308
- Palmer JH, Ball DR. The effect of cricoid pressure on the cricoid cartilage and vocal cords: an endoscopic study in anaesthetized patients. Anaesthesia 2000;55:253–8. PMID: 10671846
- Smith CE, Boyer D. Cricoid pressure decreases ease of tracheal intubation using fiberoptic laryngoscopy. Can J Anesth 2002; 49(6): 614-9. PMID: 12067876
- Oh J et al. Videographic analysis of glottic view with increasing cricoid pressure. Ann of EM 2013; 61: 407-13. PMID: 23306455
- Fenton PM, Renolds F. Life-saving or ineffective? An observational study of the use of cricoid pressure and maternal outcome in an African setting. Int J Obstet Anes 2009; 18: 106-110. PMID: 19144507
Post Peer Reviewed By: Salim R. Rezaie, MD (Twitter: @srrezaie)
The post Cricoid Pressure in Airway Management: The IRIS Trial appeared first on REBEL EM - Emergency Medicine Blog.
