
Background Information:
 Refractory out of hospital cardiac arrest (OHCA) is defined as prolonged cardiac arrest and cardiac arrest without return of spontaneous circulation (ROSC). In addition to an already morbid condition, the chances of these patients surviving drops below 5% when cardiopulmonary resuscitation (CPR) is performed during transport to the hospital.1 A proposed solution is the replacement of the patient’s failed circulatory system using extracorporeal life support during CPR (ECPR) but this has only been studied in one smaller randomized control trial before called the ARREST Trial (reviewed previously on REBEL EM here). The authors of this study wanted to investigate the benefit of early intra-arrest transport and invasive interventions like ECPR on neurologic outcomes when compared to standard therapy for refractory OHCA
Refractory out of hospital cardiac arrest (OHCA) is defined as prolonged cardiac arrest and cardiac arrest without return of spontaneous circulation (ROSC). In addition to an already morbid condition, the chances of these patients surviving drops below 5% when cardiopulmonary resuscitation (CPR) is performed during transport to the hospital.1 A proposed solution is the replacement of the patient’s failed circulatory system using extracorporeal life support during CPR (ECPR) but this has only been studied in one smaller randomized control trial before called the ARREST Trial (reviewed previously on REBEL EM here). The authors of this study wanted to investigate the benefit of early intra-arrest transport and invasive interventions like ECPR on neurologic outcomes when compared to standard therapy for refractory OHCA
Paper: Belohlavek J, et al. Effect of Intra-arrest Transport, Extracorporeal Cardiopulmonary Resuscitation, and Immediate Invasive Assessment and Treatment on Functional Neurologic Outcome in Refractory Out-of-Hospital Cardiac Arrest: A Randomized Clinical Trial. JAMA. 2022 Feb 22, 2022 PMID: 35191923
Clinical Question:
- In patients with witnessed refractory OHCA, does early intra-arrest transport, ECPR and immediate invasive assessment and treatment improve neurologic outcome compared to standard resuscitation?
What They Did:
- Randomized control trial performed at a single large cardiac center in Prague, Czech Republic
- Consent was obtained from each participants legal representative as soon as possible and all patients who regained normal neurologic function were asked for written consent
- Enrollment was conducted closely with the Prague EMS dispatch center
- The study coordinator was automatically notified when the dispatch center initiated telephone-assisted bystander chest compressions
- A telephone connection was established between the coordinator and the physician or paramedic on scene.
- The coordinator then logged into a 24-hour web-based secured randomization system to assign the patient into one of two groups: either the invasive or standard strategy
-
Standard strategy: Patients received continued ACLS and received drugs, further defibrillations or other interventions that followed these standard guidelines
- If ROSC was achieved, transport was initiated and coronary angiography encouraged
-
Invasive strategy: Patients received continued ACLS and all therapies associated with those guidelines in addition to intra-arrest intranasal evaporative cooling if feasible.
- The patient was immediately transferred directly to the cardiac center’s cath lab during ongoing CPR with the intention of proceeding with ECPR if ROSC was not obtained en route or on admission
- ECMO cannulation was performed on the cath table during ongoing mechanical CPR using a femoro-femoral approach
- After diagnostic and therapeutic cath lab procedures were done an antegrade perfusion cannula was implanted under ultrasound guidance and these patients were continuously anticoagulated with heparin unless contraindicated
- Post-arrest resuscitation care was standardized in both groups and included the following:
- Close monitoring of labs
- Urgent bedside echocardiogram
- Whole-body CT scans if feasible and clinically indicated
- Targeted temperature management via intravascular or surface cooling initially to 33oC and later made 36oC following the TTM trial being published
- All other post-arrest care according to European Resuscitation Council including withdrawal of life-sustaining therapies
- A crossover from the standard to the invasive group (and vice versa) was allowed in select patients based on the request of an emergency physician
- For the standard to invasive crossover there needed at least 2 additional unsuccessful defibrillations after randomization
- Invasive to standard crossover occurred when continuing care with invasive measures was deemed to be futile
- Lastly, to measure favorably neurologic outcome, the study authors utilized the Cerebral Performance Category (CPC) Score (Figure 1) and had both groups assessed by a neurologist in a blinded fashion

Figure 1: Cerebral Performance Category Scale
Inclusion Criteria:
- Adults aged 18 to 65 years old receiving ongoing resuscitation for witnessed OHCA of presumed cardiac etiology who had received a minimum of 5 minutes of ACLS without ROSC
Exclusion Criteria:
- Unwitnessed cardiac arrest or presumed non-cardiac cause
- Suspected or confirmed pregnancy
- Attainment of ROSC within 5 minutes during initial resuscitation
- Regained consciousness
- Obvious life-limiting comorbidities
- Bleeding diathesis
- Known Do-Not-Resuscitate (DNR) order
- Known pre-arrest CPC of 3 or greater
Outcomes:
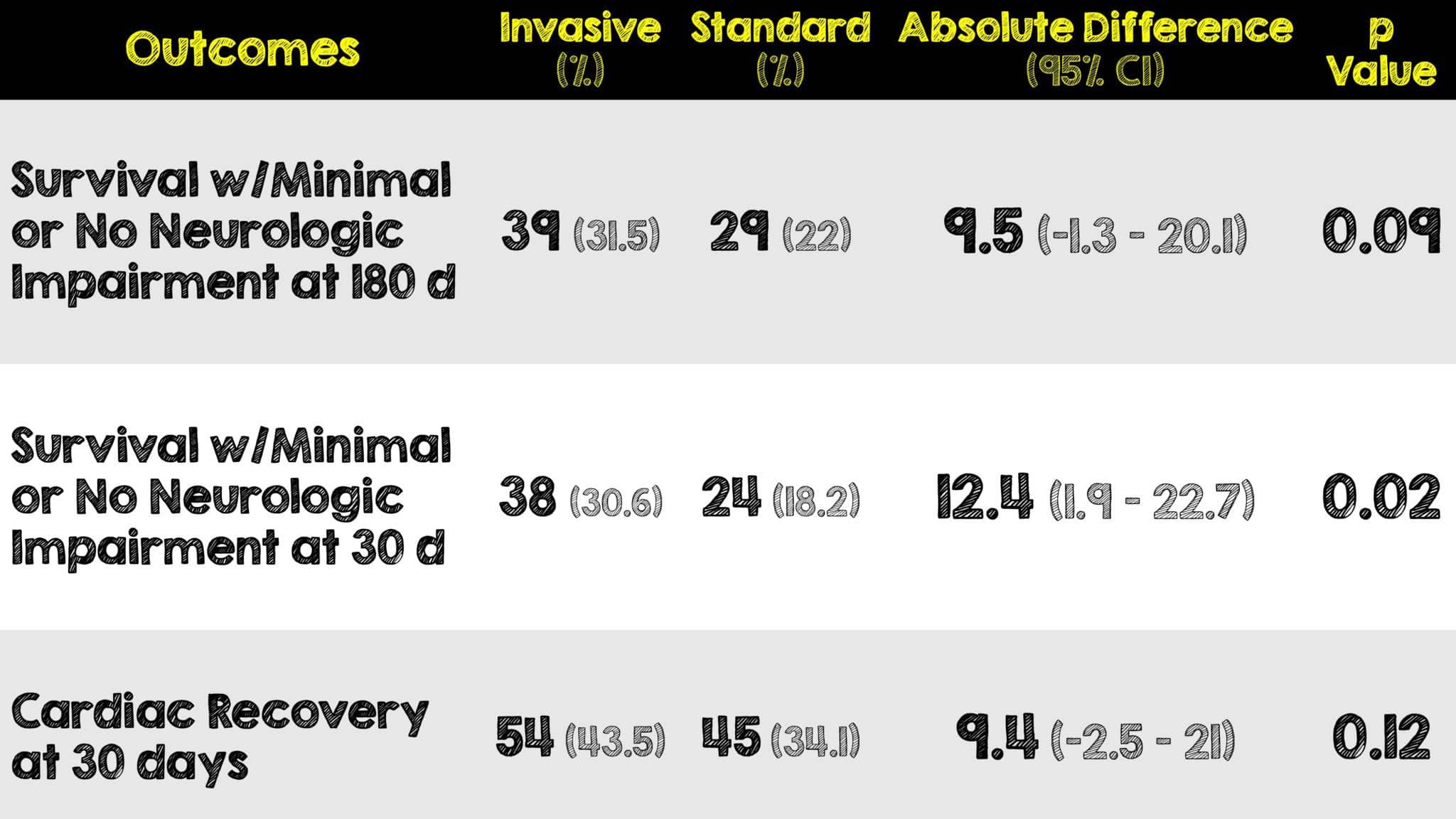
Primary
- 180-day survival with favorable neurologic outcome defined as a CPC of 1 or 2 (ie. no or minimal neurologic impairment)
Secondary
- 30-day survival with cardiac recovering (no need for pharmacological or mechanical cardiac support for 24 hours)
- Neurologic recovery (CPC 1 or 2) at any point within the first 30 days after cardiac arrest
Results:
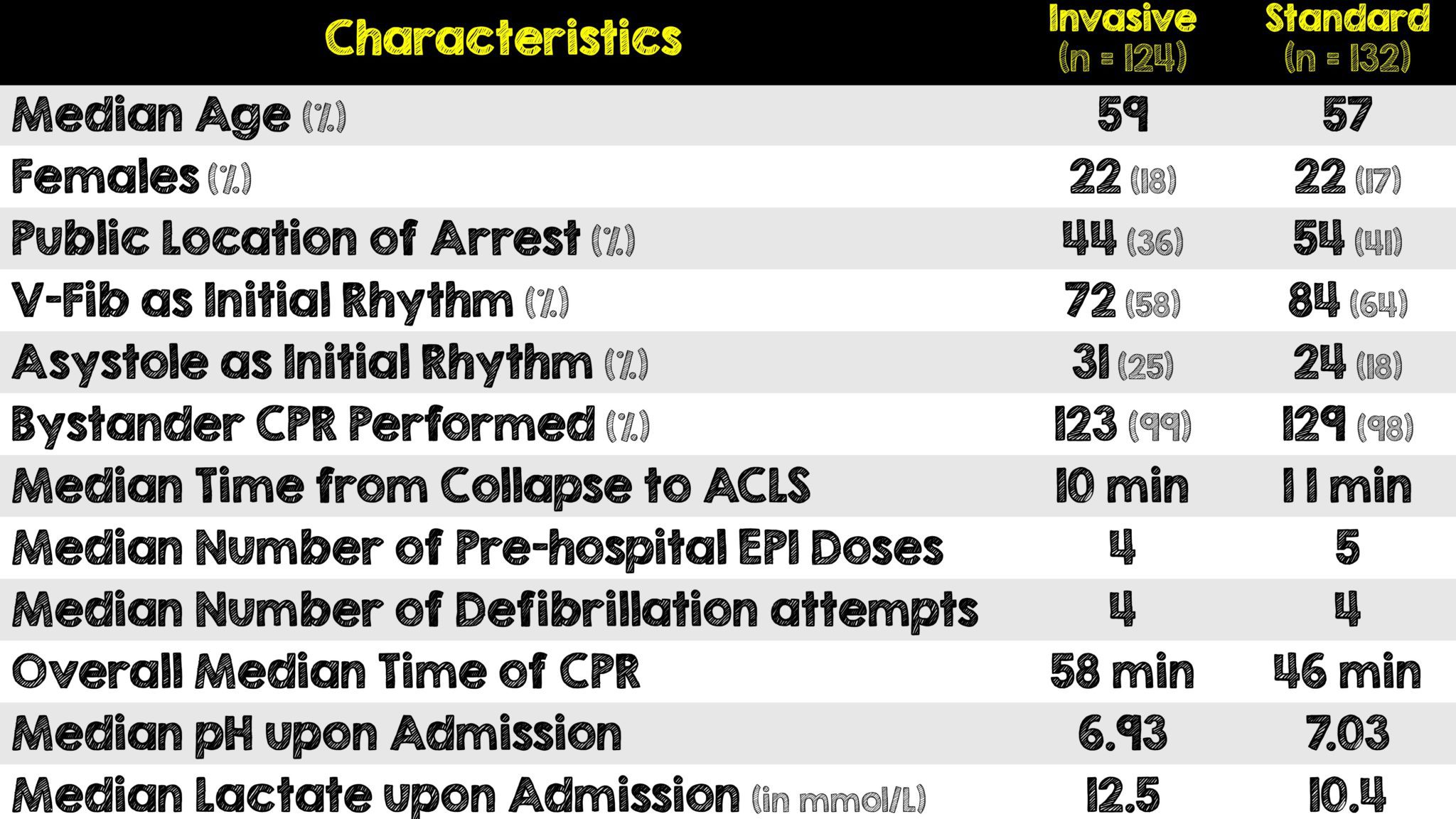
- Of the 264 eligible patients, a total of 256 were enrolled
- The study was terminated early because the standardized test statistics for results of a primary end point intersected a prespecified stopping rule for futility at 256 patients.
- There were 11 crossovers from the standard to the invasive group and 9 crossovers from the invasive to the standard group
Critical Results:
- Targeted temperature management was used in 117 of 123 (95%) of patients in the invasive group and 61 of 87 (70%) of the patients in the standard group
- Immediate PCI was performed successfully in 56/62 (90%) of patients in the invasive group and 24/30 (80%) in the standard group
- 11 of 124 (9%) of invasive group patients were declared dead on scene/during transport or within one hour of admission compared with the 64 of 132 (49%) standard group patients
- Bleeding occurred more frequently in the invasive (31%) vs standard strategy group (15%)
Strengths:
- First study assessing the use of ECMO during on-scene ongoing CPR
- All 256 (100%) of patients completed the trial with no loss to follow-up
- Neurologic outcomes were determined by a neurologist that was blinded to randomization
- Coordination with Prague EMS dispatch center to set up consecutive as opposed to convenience sampling for patient enrollment
- Although these were witnessed arrests, bystander CPR was performed in 252 out of 256 (98%) of the patients which is an incredibly high amount of good-Samaritans
- Utilized a truly multidisciplinary approach to critical care in getting patients cannulated while on the cath lab
- Adjusted practice as new evidence and data emerged on therapies (ie. mechanical CPR and TTM)
- Kept intra-arrest interventions (ie. ACLS, drugs, defibrillation) and post-arrest care (ie. TTM, TTE, CT and Neuro-prognostication) the same across both groups
- EMS response time paralleled that found in well-developed countries (ie. 7 to 8 min)2
- Primary outcome was a clinically relevant patient-oriented outcome with no missing data for its analysis
Limitations:
- Single academic center in a single country thus limiting external validity
- Limited enrollment looking at only witnessed cardiac arrest from cardiac etiology
- Underpowered sample size (due to early termination of trial) to detect a statistically significant difference for the primary outcome
- Excluded patients with unwitnessed cardiac arrest and patients with non-cardiac cause of their arrest
- Emergency physicians on many ambulances helps enforce standard practices and adherence to guidelines is not found in many other places in the world (ie. United States)
- Majority of institutions are not ECMO centers and do not have as extensive intra-arrest and post-arrest care capabilities (more on this below)
- Priori scenarios of expected benefit from the invasive strategy were not reached likely due to the higher-than-expected survival in the standard strategy group.
- Allowed crossover between the two groups due to EMS transporting of patients
- Trial terminated early and thus results may be overestimated or in this case underestimated
Discussion:
- The authors should be applauded for performing this trial as there is limited information in the literature regarding ECPR. The only other study was the ARREST Trial (which again we covered before on REBEL here) showed that ECPR improved survival to hospital discharge and functional status compared to patients receiving standard therapy. Unlike this study, it only included patients with shockable rhythms and only those who were transferred to the hospital were randomized (following approximately 50 minutes of CPR).3
- Part of the reason crossover was allowed in this study is because EMS crews transported some patients receiving ongoing CPR for ECPR despite being randomized to the standard therapy group.
- Although there was a low rate of crossover compared to other studies, the rejection of patients in receiving advanced therapies introduces a degree of subjectivity and bias which was not definitively measured and ultimately could influence outcomes
- 64% of the patients in this study experienced cardiac arrest longer than 45 minutes. Under the same conditions, there are not many institutions or EMS agencies in the United States that would run a code this long. It’s unclear if this is standard practice in Prague, the result of such high bystander CPR, the impact of telephone-assisted CPR or if this was intentionally done by biased providers knowing these patients were being enrolled in a study looking at neurologic outcome
- Ability to perform PCI or any other cath procedures while active CPR is ongoing just doesn’t happen at most hospitals (procedures like those are usually terminated, not continued and certainly not initiated, because of cardiac arrests)
- It’s worth noting that the invasive strategy group was sicker than the standard strategy group as noted by them having a lower pH and higher lactate on admission. This could have been because they received a longer amount of CPR time as every effort was made to bring these patients to the hospital’s cath lab
- The invasive strategy group also had more ECPR complications such as major bleeding events. In addition to being underpowered, this combined with the longer duration of CPR leading to sicker patients may or may not have contributed to why there was no appreciable difference seen
- An ongoing question remains: when should ECPR be initiated during cardiac arrest?
- In this study, it was following 16 minutes of professional on scene CPR which the authors advocate as a “satisfactory approach to select truly refractory cases”
- The question of when to initiate ECPR may be better answered by asking WHOM prognostically should this invasive intervention be performed
Author’s Conclusions:
- Among patients with refractory out-of-hospital cardiac arrest, the bundle of early intra-arrest transport, ECPR, and invasive assessment and treatment did not significantly improve survival with neurologically favorable outcome at 180 days compared with standard resuscitation. However, the trial was possibly underpowered to detect a clinically relevant difference.
Our Conclusion:
- Although terminated early, this study helps bring questions related to the timing and patient selection of ECPR into the limelight to be further studied. Unfortunately, the system in which this study was performed is incredibly unique in many ways and far from where the majority practice making it difficult to directly apply the results of this single center trial.
Clinical Bottom Line:
- This underpowered single center study was terminated early however the use of ECPR may have promising results in future studies if the timing and appropriate patients are selected. It will likely require multiple system-wide factors such as a high rate of bystander CPR, a well-developed EMS system and a progressive multidisciplinary team of specialists providing intensive intra-arrest critical care at specialized cardiac centers.
Expert Opinion and Interview

Frank Guyette, MD, MS, MPH, FACEP, FAEMS
Professor of Emergency Medicine
Medical Director, STAT MedEvac
Post-Cardiac Arrest Service Attending
University of Pittsburgh Medical Center
Belohlavek et al. present the results of an eight-year effort to determine whether an early invasive approach in adults with refractory OHCA improves neurologically favorable survival. They enrolled 256 subjects between 18-65 years old receiving ongoing resuscitation for witnessed cardiac arrest that had received a minimum of 5 minutes of ACLS without ROSC when the ECPR team was available. One hundred twenty-four were randomized to the invasive strategy group and 132 were in the standard strategy group. Among patients with the bundle of early intra-arrest transport, ECPR and invasive assessment and treatment without improvement in survival with neurologically favorable outcome at 180d.
This is an incredibly challenging study which required heroic effort and coordination sustained over many years. While they did not reach significance on their primary outcome (180 survival w/good neurologic outcome) the point estimates are similar to other studies of ECLS for the invasive group while the survival in the standard treatment group was much higher (22%) than the 10% assumed by the sample size calculation. The secondary outcome of neurologic recovery at 30 days was significant. Furthermore, specific issues regarding this study design may have contributed to this outcome. The effect size was a relative ~63% odds of improvement in the primary outcome despite not reaching significance. There is risk of a type II error. In addition, the study did not exclude patients with non-shockable rhythms which may have biased it to the null given the lower likelihood of survival and reversible cause in that group. Using exclusion criteria such as presumed non-cardiac cause is open to interpretation and may have contributed to a patient population less likely to benefit from invasive therapy. The intervention also occurred over a long period of time with changing technology in resuscitation which may have introduced secular trends that contributed to the higher survival in the standard cohort.
Do you feel the difference in EMS systems played a big role in the methodology or the results of this trial? If so, how?
- Successful implementation of an ECLS trial cannot occur without a robust EMS system. Rapid identification of candidates for the therapy, high quality prehospital resuscitation, notification systems and coordination of care are all a must for any successful ECPR effort. Having a mature system is critical. If you can’t provide high quality basic ACLS then it is a nonstarter. Having a physician in the field can be a benefit or a hinderance, but in this case someone tasked for patient screening/identification and acting as a champion is important. These are rare events (<3 a month) so vigilance is important. Timely communication with the hospital and EMS dispatch system requires a high degree of coordination.
What is the timing and patient selection criteria for ECPR in Pittsburgh?
- …ECPR in Pittsburgh requires that the paramedics identify an arrest that is witnessed, with a shockable rhythm (VT/VF) in a patient <=65 y/o with a high level of premorbid function. This patient is identified for ECPR if they have had 3 unsuccessful shocks (refractory VF). At that point they are extricated from the scene on a LUCAS and transported to either Pittsburgh’s main quaternary hospital (PUH) or Allegheny General Hospital (AGH, the other major health system in the city), whichever is closer. Upon arrival at the trauma bay (PUH) or cath lab (AGH) they are met by the ECMO team which evaluates the patient for suitability of ECMO and can be cannulated within 50 min if cannulation is feasible (habitus, concomitant PVD), and is there no other history that would preclude cannulation (metastatic disease or DNR).
In regards to neurologic outcomes and prognostication following cardiac arrest, should the authors have used the CPC Score? Why or why not?
- …The Cerebral Performance Category (CPC) is useful because it can be calculated easily from the patient record or disposition information. It was described by Jennet and Bond in 1975 further described by Peter Safar (1981) and is associated with long term patient outcomes and modified Rankin Scale. It is widely used as a surrogate for neurologic outcome in resuscitation studies. Other scales may be more comprehensive, but they require arduous prospective collection.
Where do you see the future of ECPR going after this study?
- …ECPR requires coordinated approaches to reach a very narrow subset of the population that benefits. Health care systems (911 centers, EMS services, hospitals etc) need to be built around cardiac arrest much like trauma centers. Once we have created the infrastructure for high quality CPR, and the coordinated wrap around services proven to increase survival, then ECPR can flourish. For the time being that will be limited to a few academic centers.
REFERENCES:
- Belohlavek J, et al. Effect of Intra-arrest Transport, Extracorporeal Cardiopulmonary Resuscitation, and Immediate Invasive Assessment and Treatment on Functional Neurologic Outcome in Refractory Out-of-Hospital Cardiac Arrest: A Randomized Clinical Trial. JAMA. 2022 Feb 22, 2022 PMID: 35191923
- Mell HK, Mumma SN, Hiestand B, Carr BG, Holland T, Stopyra J. Emergency Medical Services Response Times in Rural, Suburban, and Urban Areas. JAMA Surg. 2017 PMID: 28724118
- Yannopoulos D, et al Advanced reperfusion strategies for patients with out-of-hospital cardiac arrest and refractory ventricular fibrillation (ARREST): a phase 2, single centre, open-label, randomised controlled trial. Lancet. 2020 Dec 5, PMID: 33197396
For More Thoughts on This Topic Checkout:
- REBEL EM: The ARREST Trial: ECMO or EC-No
- First10inEM: The ARREST Trial – ECMO CPR
- The Bottom Line: ARREST Trial
Post Peer Reviewed By: Salim Rezaie, MD (Twitter: @Srrezaie)
The post Effect of Intra-Arrest Transport and eCPR on Neurologic Outcomes in Refractory OHCA appeared first on REBEL EM - Emergency Medicine Blog.
