
 Anaplasmosis
Anaplasmosis
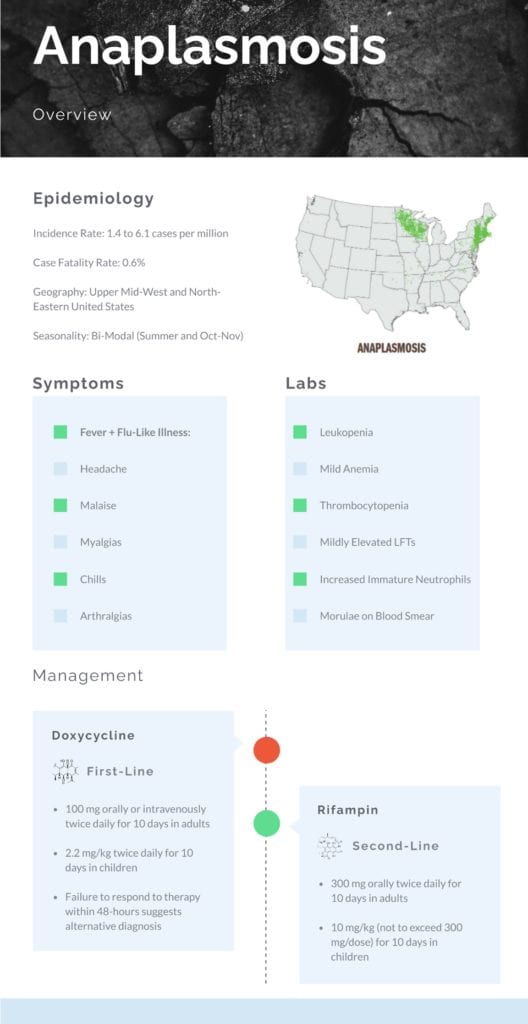
Epidemiology
Incidence:
- Overall annual incidence rose from 1.4 to 6.1 cases per million in the United States between 2000 and 2010 (Ismail 2017)
- In endemic areas, the incidence rate is suggested to be more than 50 cases per 100,000 (Ismail 2017)
Age:
- Median age is 51 years of age with greater than 95% of cases reported in Caucasian patients (Ismail 2017)
Gender:
- Slight male to female predominance (Demma 2006)
Morbidity/Mortality: Case fatality rate is less than 1% (Ismail 2017)
- Many patients will be either asymptomatic or manifest mild signs and symptoms
- Hospitalization rates have been noted to be as high as 36% in epidemiological studies with a 7% ICU admission rate and mortality rate of 0.6% in those with severe symptoms (Dumler 2012)
Geography and Seasonality (Baker 2020): Upper Midwestern and Northeastern United States
- Ten States account for over 90% of all reported cases (in order from highest concentration of cases): Minnesota, Wisconsin, Massachusetts, New York, Maine, Connecticut, New Jersey, Rhode Island, Vermont, and New Hampshire.
- Seasonal distribution is concentrated in summer months corresponding to nymphal tick activity: June (23.4%), July (22.2%), August (12%), and May (10.4%).
- Second smaller peak is noted in October and November when adult ticks are active
Poor Prognostic Factors:
- Increased Age
- Immunocompromised States
- Delays in diagnosis and treatment
Pathogenesis (Biggs 2016):
- After tick transmissibility, Anaplasma phagocytophilum has a predilection for granulocytes, specifically neutrophils
- Once infected, the organism multiplies within cytoplasmic membrane-bound vacuoles forming clusters of bacterial called morulae
- Infection elicits a systemic inflammatory response and alters the host’s neutrophil function leading to ineffective inflammatory regulation and microbicidal activity
History and Physical:
Symptoms (Ismail 2017, Biggs 2016):
- Symptoms typically appear 5-14 days after bite of an infected tick
- Rash is present in less than 10% of patients
- Fever occurs in 92-100% of recognized cases of anaplasmosis along with other non-specific flu-like symptoms:
- Headache
- Malaise
- Myalgias
- Chills/Rigors
- Arthralgias
- Gastrointestinal symptoms are less frequently seen
- Central Nervous System involvement is rare
- Severe Manifestations: Most cases are self-limiting, but Anaplasmosis has been associated with the following severe disease manifestations:
- ARDS
- DIC
- Rhabdomyolysis
- Renal Failure
- Pancreatitis
- Hemophagocytic Syndromes
- Opportunistic Viral and Fungal infection
Diagnosis:
Labs: Characteristic laboratory findings are seen in Anaplasmosis along fever and non-specific flu-like illness:
- Leukopenia
- Mild Anemia
- Thrombocytopenia
- Mild to Moderate Elevated Hepatic Transaminase
- Increased Number of Immature Neutrophils
Blood Smear:
- May see morulae within granulocytes with microscopic examination of blood smears but blood smear may be relatively insensitive and inconsistent and dependent on operator experience (Biggs 2016)
- Observation of morulae is highly suggestive of infection
Confirmatory Testing (Ismail 2017):
- Serological testing of IgM and IgG antibodies specific to A phagocytophilum using indirect immunofluorescence assay (IFA) is the gold standard.
- RT-PCR assays are also available for diagnosis of A phagocytophilum and has become the test of choice due to rapid turnaround times and high specificity as well as sensitivity
Guest Post By:

Akash Ray, DO
PGY-2 Emergency Medicine Resident Inspira Medical Center
Vineland, NJ
Twitter: @_kashray
References:
- Biggs H et al. Diagnosis and Management of Tickborne Rickettsial Diseases: Rocky Mountain Spotted Fever and Other Spotted Fever Group Rickettsioses, Ehrlichioses, and Anaplasmosis – United States. MMWR Recomm Rep. 2016. PMID: 27172113
- Todd S et al. No visible dental staining in children treated with doxycycline for suspected Rocky Mountain Spotted Fever. J Pediatr. 2015. PMID: 25794784
- Volovitz B et al. Absence of tooth staining with doxycycline treatment in young children. Clin Pediatr (Phila). 2007. PMID: 17325084
- Ismail N et al. Tick-Borne Emerging Infections: Ehrlichiosis and Anaplasmosis. Clin Lab Med. 2017. PMID: 28457353
- Demma L et al. Human monocytic ehrlichiosis and human granulocytic anaplasmosis in the United States, 2001–2002. Ann N Y Acad Sci. 2006. PMID: 17114690
Post Peer Reviewed By: Salim R. Rezaie, MD (Twitter: @srrezaie)
The post Emerging Tick-Borne Illnesses: Not Just Lyme Disease Part 2 Anaplasmosis appeared first on REBEL EM - Emergency Medicine Blog.
