Background Information:
 Multiple illness severity scores have been developed for use after out-of-hospital cardiac arrest (OHCA) and in-hospital cardiac arrest (IHCA). Unfortunately, these rely on information that is not immediately available to providers in the early hours following return of spontaneous circulation (ROSC).1 The Pittsburgh Cardiac Arrest Category (PCAC) Score (Figure 2) was derived from the Full Outline of UnResponsiveness (FOUR) brainstem and motor sub-scores (Figure 1). It also uses the cardiac and respiratory subscales from the SOFA Score. PCAC was created to be a simple scoring system that focused on objective physical findings for immediate post-arrest prognostication.2 The Pittsburgh group internally validated the score finding it a useful method for making early estimates of prognosis.3 Now the post cardiac arrest service at the University of Alabama at Birmingham sought to externally validate the PCAC severity score.
Multiple illness severity scores have been developed for use after out-of-hospital cardiac arrest (OHCA) and in-hospital cardiac arrest (IHCA). Unfortunately, these rely on information that is not immediately available to providers in the early hours following return of spontaneous circulation (ROSC).1 The Pittsburgh Cardiac Arrest Category (PCAC) Score (Figure 2) was derived from the Full Outline of UnResponsiveness (FOUR) brainstem and motor sub-scores (Figure 1). It also uses the cardiac and respiratory subscales from the SOFA Score. PCAC was created to be a simple scoring system that focused on objective physical findings for immediate post-arrest prognostication.2 The Pittsburgh group internally validated the score finding it a useful method for making early estimates of prognosis.3 Now the post cardiac arrest service at the University of Alabama at Birmingham sought to externally validate the PCAC severity score.
Paper: Nassal MMJ, et al. External validation of Pittsburgh Cardiac Arrest Category illness severity score. Resuscitation. 2022 Mar; 17. PMID: 34968531
https://rebelem.com/wp-content/uploads/2022/06/External-Validation-of-PCAC-Figure-1.5-300x169.jpg 300w, https://rebelem.com/wp-content/uploads/2022/06/External-Validation-of-PCAC-Figure-1.5-1024x576.jpg 1024w, https://rebelem.com/wp-content/uploads/2022/06/External-Validation-of-PCAC-Figure-1.5-768x432.jpg 768w, https://rebelem.com/wp-content/uploads/2022/06/External-Validation-of-PCAC-Figure-1.5-1536x864.jpg 1536w, https://rebelem.com/wp-content/uploads/2022/06/External-Validation-of-PCAC-Figure-1.5-600x338.jpg 600w" height="281" width="500" class="aligncenter wp-image-16107" decoding="async">
Figure 1: Full Outline of UnResponsiveness (FOUR) Score
https://rebelem.com/wp-content/uploads/2022/06/External-Validation-of-PCAC-Figure-2-300x169.jpg 300w, https://rebelem.com/wp-content/uploads/2022/06/External-Validation-of-PCAC-Figure-2-1024x576.jpg 1024w, https://rebelem.com/wp-content/uploads/2022/06/External-Validation-of-PCAC-Figure-2-768x432.jpg 768w, https://rebelem.com/wp-content/uploads/2022/06/External-Validation-of-PCAC-Figure-2-1536x864.jpg 1536w, https://rebelem.com/wp-content/uploads/2022/06/External-Validation-of-PCAC-Figure-2-600x338.jpg 600w" sizes="(max-width: 500px) 100vw, 500px">
Figure 2: Pittsburgh Post-Cardiac Arrest Category Severity Score
Clinical Question:
- Does the Pittsburgh Cardiac Arrest Category predict survival to hospital discharge and favorable outcomes similar to original foundational models?
What They Did:
- A secondary analysis of quality improvement data maintained by the University of Alabama Birmingham Post-Cardiac Arrest Service
- Reviewed all data for OHCA and IHCA patients between 7/2009 and 7/2016
- Retrospectively calculated patient’s PCAC Score based on chart review
- The post-cardiac arrest service is a group of multi-specialty attending physicians with expertise in post-arrest care that quickly work to mobilize dedicated equipment and resources for standardized goal-directed care of post arrest patients
Inclusion Criteria:
- Adult patients > 18 years of age
- Obtained ROSC following OHCA or IHCA
- Had records adequate for analysis within the first 6 hours after cardiac arrest
Exclusion Criteria:
- Patients with incomplete data
Outcomes:
Primary
- Survival to hospital discharge
Secondary
- Discharge disposition
- Home (considered favorable)
- Acute rehabilitation (considered favorable)
- Nursing facility
- Hospice
- Death
- Discharge Cerebral Performance Category (CPC) Score
- Score of 1 or 2 considered favorable
- Discharge modified Rankin Scale
- Score of 0 – 3 considered favorable
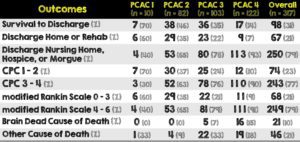
Results:
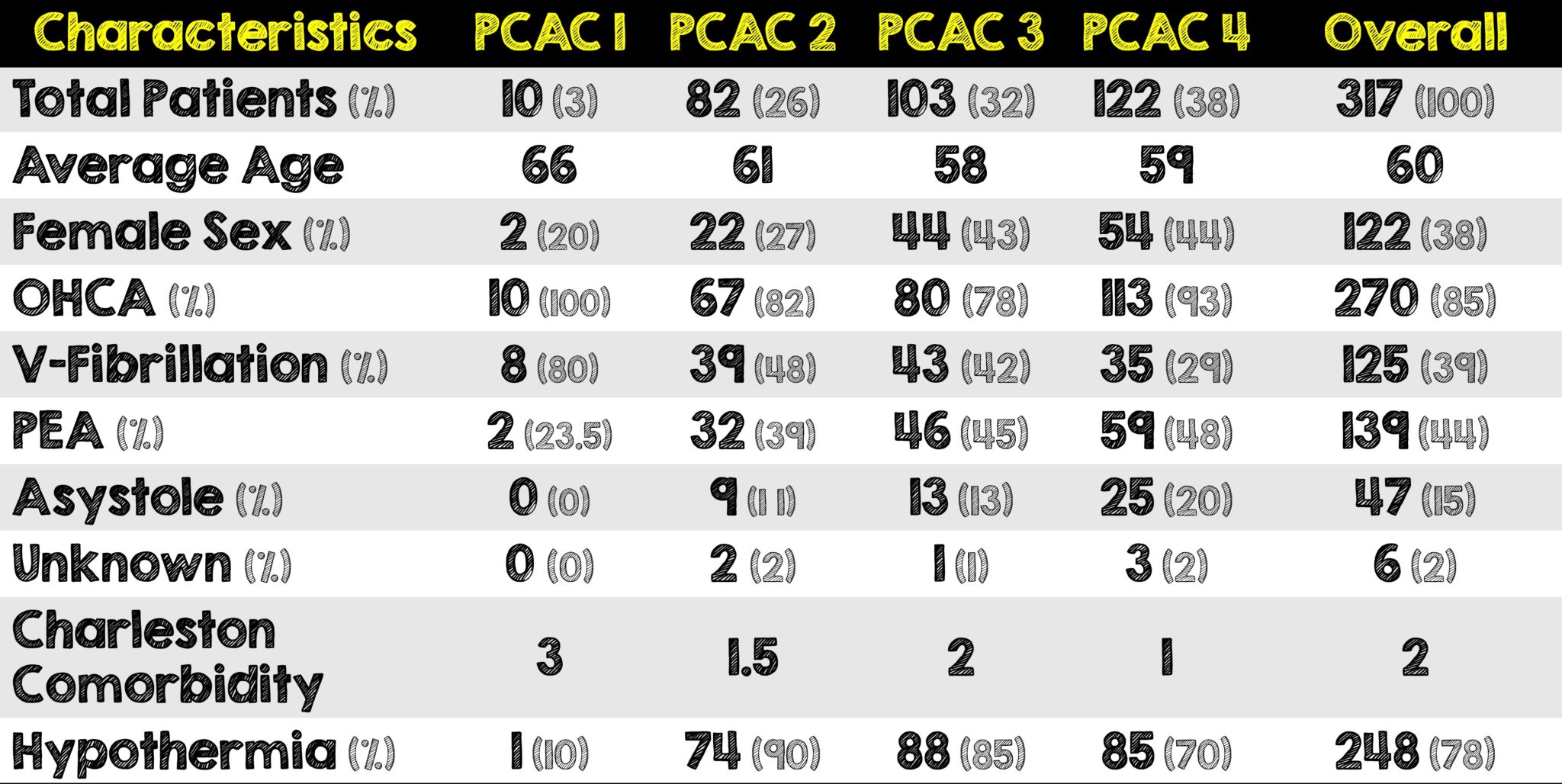
Critical Results:
Strengths:
- PCAC scoring is simple and relies on four easily attainable variables immediately within 6 hours of a post-arrest patient achieving ROSC
- Included both OHCA and IHCA
- Evaluated for patient oriented primary and secondary outcomes
- Utilized more than one quality of life scoring system (ie. CPC and mRS)
- Reviewed patients during the same time period as the internal validation paper
- Post cardiac arrest consult service follows close to 100% of cardiac arrest patients
Limitations:
- Retrospective chart review and calculation of the score
- Performed at a single institution in a single country with a specific patient population
- UAB’s entire post cardiac arrest service is modeled after Pittsburgh’s which may have introduced some implicit or unconscious bias
- Although TTM was used, it’s unclear how many patients were maintained at this temperature. Its also unclear how many had complications and how many had fever
- Majority of patients were OHCA and not IHCA (270 vs 47, respectively) thus limiting applicability to IHCA
- Very limited number of institutions have a dedicated post-cardiac arrest team and thus findings many be difficult to apply to community facilities with limited resources
- First six hours following ROSC is dynamic resulting in multiple PCAC score changes
- SOFA Cardiac component of PCAC scoring varies depending on the vasopressor initiated
- Cardiac arrest survival significantly higher than reported national average since its reported only from patients who obtain ROSC and thus leading to the overestimation of survival from all OHCA
- The authors do not mention how and who did the chart review. In post-arrest the data collected can surprisingly vary depending on whether it was a research assistant, medical student, intern, resident, fellow, etc.
Discussion:
- This post-cardiac arrest team is a consultant service that typically follows post-cardiac arrest patients from admission to hospital discharge. While the combination of their presence and a high-volume cardiac arrest center does lead to improved outcomes,4,5 the reality is that not many hospitals nationally, and arguably globally, have this kind of service readily available.
- During this study’s time period, the American Heart Association’s guideline recommendations on post-cardiac arrest care changed twice. The authors note that this did not result in changes to their institution’s hypothermia treatment goals
- Although the authors stated they reviewed patients within the same time period as the original foundational paper and the internal validation paper, this is not true. The original foundational paper looked at patients from 1/2005 to 12/2009, whereas this study started their 7-year review of patients on 7/2009.
- Depending on the vasopressor utilized, a PCAC score can vary for similar cardiac injuries. This is a major flaw in PCAC and should warrant some kind of revision for more standardization as it could mean the difference between two categories.
- It’s always important to remember not to hone in on only one severity score. Similar to looking at a multitude of data when assessing patients for additional therapies (ex. Volume assessment before giving fluids). For these complex patients, multiple variables need to be assessed to anticipate what their functional outcome will be like following their arrest. Other scores that should be considered in conjunction with PCAC. Unlike the risk-stratifying score of the PCAC, there are others that focus on outcome measures such as the 41 Cent Test and Montreal Cognitive Assessment (MoCA).6
- There is also another category of PCAC which was not mentioned in this paper and that’s those who are “Untypable”. These include patients with intracranial bleeding, hemorrhagic arrest and cardiac arrest related to substance abuse. In Pittsburgh, a place that sees over 300 cardiac arrests a year, roughly 10-15% of these patients are PCAC Untypable.
- Cardiac arrest illness severity is heterogeneous and dynamic thus obscuring more accurate early prognosis. Assigning a patient a single PCAC score upfront may implicitly bias clinicians familiar with the score in how they care for patients. This becomes even more problematic if a patient was made a PCAC III as opposed to a PCAC II simply because of the vasopressor chosen or if they made significant improvements immediately after being scored.
- Talking with the Pittsburgh Post-Cardiac Arrest service, they say that the PCAC score was not meant to be dynamic. Similar to how a patient’s Hunt and Hess Score (for Subarachnoid Aneurysm) doesn’t change once assigned to a patient. Yet, this may contribute to an implicit bias. A possible way around this, in addition to modifying it for better standardization, is to reassess the patient’s PCAC score at a set time period (ie. 12 or 24 hours) and utilizing the best of the two scores.
- An example using a real case I had while on call in the ICU:
- A 61-year-old female had a post-induction arrest on the wards/hospital telemetry floor after being intubated for airway protection. She achieved ROSC, was not moving any of her extremities, or following commands. Her pupillary and corneal reflexes were absent, cough and gag present. She had a FOUR score of 1. Cardiogenic shock was suspected based on a physical exam, POCUS assessment and her minimal response to 0.3 mcg/kg/min of Norepinephrine an hour following ROSC.
- At this point her PCAC score would be 4. An hour later, the norepinephrine was able to be weaned off after she was put on dobutamine and was now moving all four extremities non-purposefully, technically making her PCAC Score 2.
- This patient just went from an overall survival of 10% to 60% but would be labeled a PCAC Score of 4 during her entire recovery when that may not be the most accurate initial assessment.
- This scoring system does have significant utility when determining what treatments or interventions certain categorized patients receive. In Pittsburgh, patients who are PCAC 4 are protocolized to receive 33oC and their neuro-resuscitation may be prioritized over other interventions such as the cath lab. The concern here is that the use of this score results in a self-fulling prophecy where we think patients are not doing well because we have already categorized them before any appropriate interventions
- The next larger-scale step to take would be to see what outcome certain PCAC patients have from these interventions and/or the lack of certain tests/imaging due to their category. Lastly if said studies were to be performed then operationalized, healthcare costs could be dramatically altered based on these findings.
Author’s Conclusions:
- Early (<6 h post-arrest) PCAC severity scoring strongly predicts patient outcomes from cardiac arrest in both OHCA and IHCA.
Our Conclusion:
- The PCAC score is simple, quick to use and may play a role in post-cardiac arrest assessment and provide additional information regarding neuro-prognostication. Due to the dynamic nature of these critically ill patients, the discrepancy based on vasopressor selection and anchoring bias, the use of this score should be considered keeping in mind these limitations. The next step in the utility of this score would be assessing the outcomes of patients in specific categories when certain interventions are performed or simply not offered.
Clinical Bottom Line:
- While the external validation of the simple and quick to use PCAC score is promising, post-cardiac arrest patients are dynamic and the use of this score should be done after understanding it’s limitations. The bigger question that remains unanswered is how are the outcomes of patients in specific categories are impacted when certain interventions and treatments are performed versus withheld. Lastly, there’s some concern that the use of this score can cause a self-fulfilling prophecy where sicker patients do worse because we withhold certain interventions and never give them a chance to improve based on what category we put them in.
REFERENCES:
- Nassal MMJ, et al. External validation of Pittsburgh Cardiac Arrest Category illness severity score. Resuscitation. 2022 Mar; 17. PMID: 34968531
- Rittenberger JC, et al. An early, novel illness severity score to predict outcome after cardiac arrest. Resuscitation. 2011 Nov. PMID: 21756969
- Coppler PJ, et al. Validation of the Pittsburgh Cardiac Arrest Category illness severity score. Resuscitation. 2015 Apr. PMID: 25636896
- Schober A, et al. Admission of out-of-hospital cardiac arrest victims to a high volume cardiac arrest center is linked to improved outcome. Resuscitation. Epub 2016 Jun 28. PMID: 27368428
- Elmer J, et al. Long-Term Outcomes of Out-of-Hospital Cardiac Arrest Care at Regionalized Centers. Ann Emerg Med. Epub 2018 Jul 4. PMID: 30060961
- Koller AC, et al. Comparison of three cognitive exams in cardiac arrest survivors. Resuscitation. Dec 2017. PMID: 28511984
Post Peer Reviewed By: Salim Rezaie, MD (Twitter: @srrezaie)
Expert Opinion

Dr. Ankur Doshi, MD, FACEP
Associate Professor of Emergency Medicine
Medical Student Education Coordinator
Post-Cardiac Arrest Service Attending
University of Pittsburgh Medical Center
Questions for the Expert:
- Since post-cardiac arrest is so dynamic, what are your thoughts on a second PCAC score being taken at a different time and accepting the better of the two scores?
This is a good question. PCAC has not been evaluated in a later time course (12-24 hours). We would need to see if the score is valid in that time from scratch. Not a bad idea, just not something we have done.
- Could the use of PCAC create an implicit bias in how we take care of patients/accept them from other facilities?
I think that clinical gestalt is something we all do and very prone to bias. Hopefully, clinical scores help us with this. An analogy that I use is the PERC rule or Wells’ scoring. Most of the data shows that we get away from our biases when we use scores as opposed to just our own clinical thoughts. We hope that PCAC would be similar, but I’m not sure we have enough data to be sure. I would rather use a PCAC score to decide on transfer than arrest characteristic (time of CPR, initial rhythm, etc) because we know that all of that data is prone to bias as well. Right now, we do not use PCAC in our decisions to transfer or not, by the way.
- Along those same lines, could the PCAC score be contributing to a self-fulfilling prophecy where sicker patients may not be given the chance to improve based on interventions we’ve withheld?
If we withheld therapies on patients based on PCAC, then I think that this is a possibility. Here at Pitt, we do not. As above, we take the PCAC score into account when we order our interventions and may prioritize Neuroresuscitation in a PCAC 4 over a cath without a hard indication (STEMI). In a PCAC 1 or 2, we may prioritize a cath and tolerate a couple hours without ICU Neuroresuscitation. Right now it is an individualized plan and PCAC is not the only data point we use. Saying all this, IF PCAC was the only data point someone used, I would worry about the self-fulfilling prophecy especially as some PCAC 4’s do very well with optimal care.
- For a community emergency physician who just got ROSC on a post-arrest patient, what are the most important things to prioritize before the patient goes up to the ICU?
Great question! I think that the simple things are the most important to get right – oxygenation, perfusion, determination an etiology and helping make the right choices on next steps (dispo, cath, etc). Neuroresuscitation in the ED is often as simple as making sure the vent is keeping the patient oxygenated and not over ventilating them and then starting pressors to keep some MAP threshold where you think that a patient is perfusing their brain (the specific BP number is controversial). Then, getting data to see if an intervention (cath, surgery, Neuroresuscitation, etc) is needed is helpful and then helping get the patient to that treatment.
The post External Validation of Pittsburgh Cardiac Arrest Category (PCAC) Illness Severity Score appeared first on REBEL EM - Emergency Medicine Blog.