The use of heated and humidified high flow nasal cannula (HFNC) has become increasingly popular in the treatment of patients with acute respiratory failure through all age groups. I first started using it as a pediatric intensive care fellow, but had little knowledge of how it actually worked. I noticed a few years after using it successfully in children, mainly with severe bronchiolitis, that we began to use it in the adult intensive care unit as well. It seems over the past several years many studies have come out reviewing the mechanisms of action as well as its use in a variety of conditions. In this part we will summarize how it works and for part 2 we will discuss the main indications for its use in adult and pediatric patients.
The use of heated and humidified high flow nasal cannula (HFNC) has become increasingly popular in the treatment of patients with acute respiratory failure through all age groups. I first started using it as a pediatric intensive care fellow, but had little knowledge of how it actually worked. I noticed a few years after using it successfully in children, mainly with severe bronchiolitis, that we began to use it in the adult intensive care unit as well. It seems over the past several years many studies have come out reviewing the mechanisms of action as well as its use in a variety of conditions. In this part we will summarize how it works and for part 2 we will discuss the main indications for its use in adult and pediatric patients.
Heat and humidified high flow nasal cannula or as most call it, Hi Flow Nasal Cannula (HFNC), isn’t just a standard nasal cannula cranked up to very high flow rates. It actually takes gas and can heat it to 37 o C with a 100% relative humidity and can deliver 0.21 – 1.00% fi02 at flow rates of up to 60 liters/min. The flow rate and fi02 can be independently titrated based on your patient’s flow and fi02 requirements.
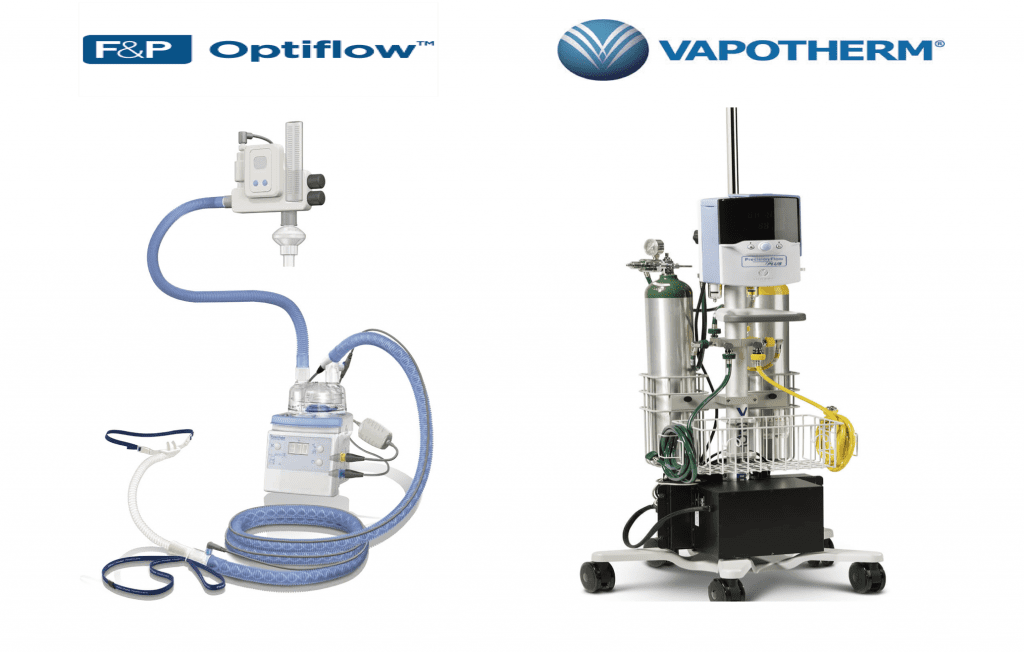
There are 2 main companies, which manufacture these devices: Vapotherm which has a device that can deliver flow rates of up to 50 liter/min flow rates and Fisher Paykall who offers both the Optiflow as well as the AIRVO 2 devices which can both deliver flow rates of up to 60 liter/min.
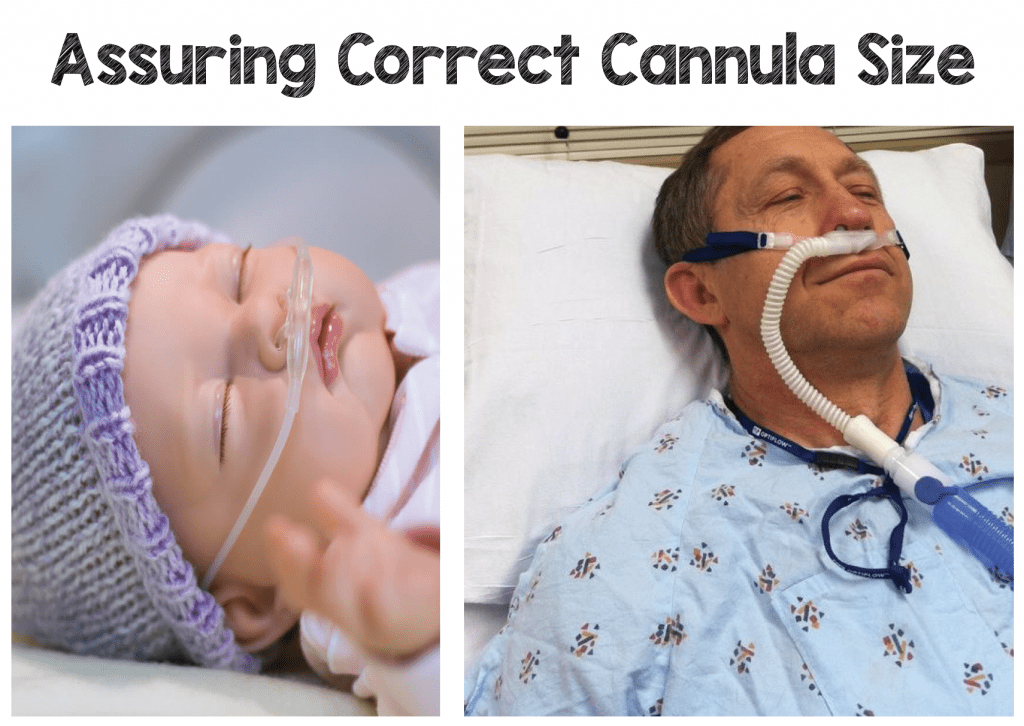
 Each company offers smaller cannula sizes for premature neonates as well as children of various ages to adult cannulas. Each cannula should snuggly fit into the patient’s nares and prevents entrainment of room air around the cannula, which can occur with standard nasal cannulas. Each manufacturer will also have a max flow rate for each cannula size corresponding to the size and age of the patient.
Each company offers smaller cannula sizes for premature neonates as well as children of various ages to adult cannulas. Each cannula should snuggly fit into the patient’s nares and prevents entrainment of room air around the cannula, which can occur with standard nasal cannulas. Each manufacturer will also have a max flow rate for each cannula size corresponding to the size and age of the patient.
How It Works:
Heated & Humidified:
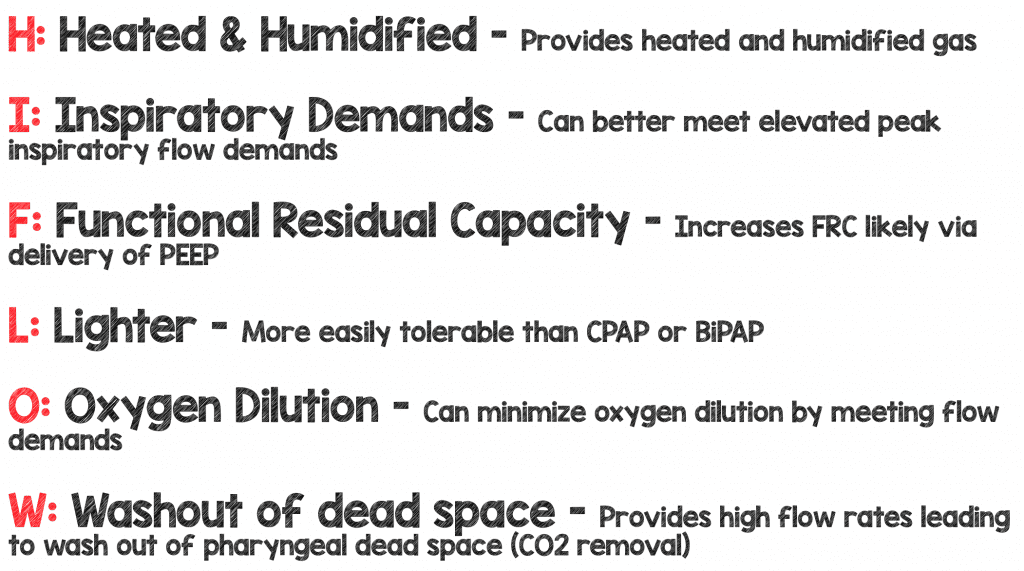
Heated and Humidified oxygen has a number of benefits compared to standard oxygen therapy. Standard oxygen therapy delivered through a nasal cannula or another device such as a non-rebreather, is cold (not warmed) and dry (not humidified). This can lead to airway inflammation, which can increase airway resistance and impair mucociliary function possibly leading to decrease secretion clearance (1). Also, a significant amount of calories can also be expended in individuals to both warm and humidify gas during normal breathing (2).
HFNC can warm (to 37oC) and humidify gas, which can decrease airway inflammation, maintain mucociliary function, improve mucous clearance and reduce the caloric expenditure in acute respiratory failure (1-2).
Inspiratory Demands:
One obvious benefit, but worth mentioning is that high flow can give you a very high flow of gas. This is important as patients in acute respiratory failure can be extremely tachypneic, and therefore their peak inspiratory flows, which may normally be 30L/min – 60L/min, can reach up to 120 L/min (3). So if you place your tachypneic patient with PIF rate of 120L/min and minute volume >20L/min on a 15L/min NRB mask, you may not be helping them as much as you think. I am going to get into this point a bit later on in this review when we discuss the concept of oxygen dilution.
Functional Residual Capacity:
You may have been looking for the bullet point that says that Hi Flow provides PEEP and you can’t find it? There has been some debate about truly how much PEEP a high flow device can deliver. HFNC has been shown to deliver up to 1 mm of Hg of PEEP for every 10L/min of flow delivered with closed mouth breathing. (4-5)
I’m not sure I believe this to be true of all patients, and this is because there are many factors that can affect how much PEEP can actually be delivered to a patient. Factors such as the patient’s size (obese, adult, child), the liter flow rate being delivered (L/Min), and mouth open versus mouth closed breathing (pressure may escape when a patients mouth is open) can all affect the amount of PEEP being delivered (4)
The debate can continue, but it does appear that HFNC can increase a patient’s functional residual volume (FRC) or the lung volume at the end of expiration something that PEEP usually improves. A study by Riera J. et al showed the use of HFNC increased End Expiratory Lung Impendence (EELI) implying there is an improvement in FRC (6). They used Electrical Impedance Tomography (EIT), a noninvasive, real-time imaging method that provides a cross-sectional ventilation image of the lung to demonstrate an increased End Expiratory Lung Impendence (EELI).
It also appears that the use of HFNC can decrease preload by increasing intra-thoracic pressure, again another feature commonly attributed to PEEP. Roca et al demonstrated in a sequential interval study on 10 patients (NYHA III Heart failure but not in an acute CHF exacerbation) that the use of Hi Flow caused inspiratory collapse of the inferior vena cava (IVC) from the patients baseline measured by echocardiogram (7).
Hi flow seems to cause alveolar recruitment and increased FRC as well as increase intrathoracic pressure likely as a result of added PEEP, however it is not certain if perhaps another mechanism may be responsible for these findings.
Lighter:
Patients often prefer the use of HFNC to that of non-invasive positive pressure ventilation (CPAP or BPAP) because the tight fitting mask can be uncomfortable to some patients. They may even prefer it to standard NC because the warmed, humidified gases won’t dry their mucosa like standard oxygen therapy (5). This may lead to higher compliance with HFNC and perhaps an improvement in your patient’s oxygenation and work of breathing.
O2 Dilution:
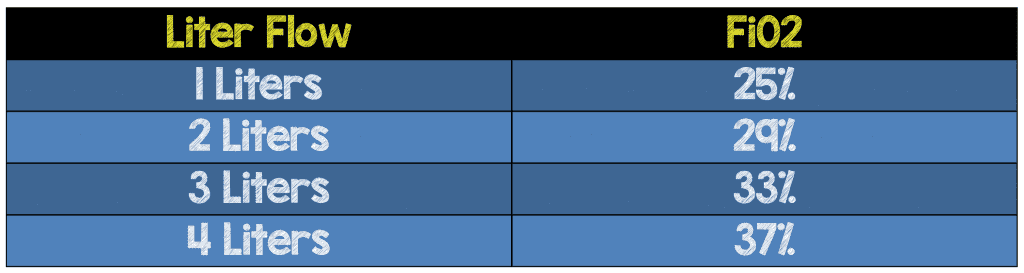
I was taught on my ICU rotation as an intern that every 1 liter of nasal cannula will deliver ~4% fiO2 above room air (21%). So 1 liter/min via the NC should deliver ~ 25% fi02, and 2 liters/min should deliver 29% fiO2 (see Table 1 below). I believed this “1:4 rule” was true for years, but let’s see if it makes sense for a patient in acute respiratory distress
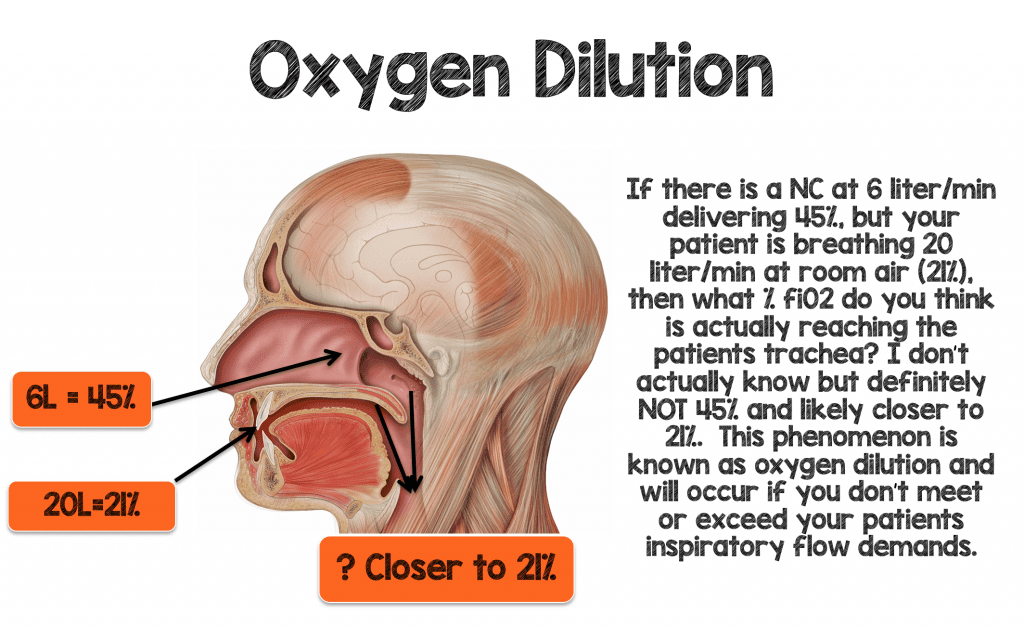
Picture a 70 kg male breathing 30-40 bpm with normal tidal volumes (~500 mL’s) and develops some hypoxemia. This patient’s minute ventilation would be between 15-20 liters/minute. You decide to place this patient on 6 liters/min NC which should theoretically deliver an fiO2 ~ 45% (6L x 4% = 24 + Room Air (21%) = 45%) if the “1:4 rule” holds true. If this patient is breathing 15-20L through his mouth and through the nares (around the nasal cannula) at 21% then do you believe that this patient will actually get 45% fiO2 delivered to the trachea?
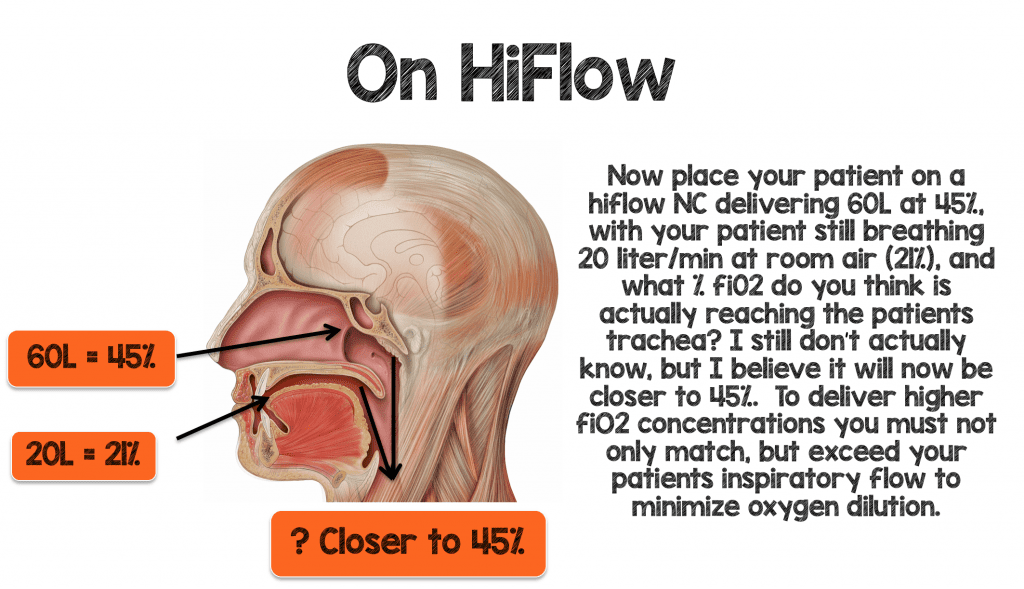
To deliver higher amounts of fiO2 effectively to your patient you have to not only match, but exceed your patient minute ventilation and inspiratory demands to minimize oxygen dilution.
Washout of Dead-space:
We normally rebreathe a third of our previously expired tidal volume and instead of breathing 21% (room air) and negligible amounts of carbon dioxide; we may rebreathe more like 15-16% oxygen and 5-6% carbon dioxide. This is because of previously exhaled breath (low in oxygen and with some carbon dioxide) is not fully exhaled and remains in the upper airway. When you patient takes their next breath from atmospheric gas not all of that gas enters the alveoli. In fact it’s a mix of the new atmospheric gas (21% 02, negligible CO2) and their previously exhaled gas (<21% oxygen and some CO2). In patients with acute respiratory failure, the percentage of gas we rebreathe gets larger, and as a result, we can rebreathe larger amounts of carbon dioxide as we draw our breaths from a mixed reservoir from our upper airway. Another way to say this is our dead-space increases with acute respiratory failure.
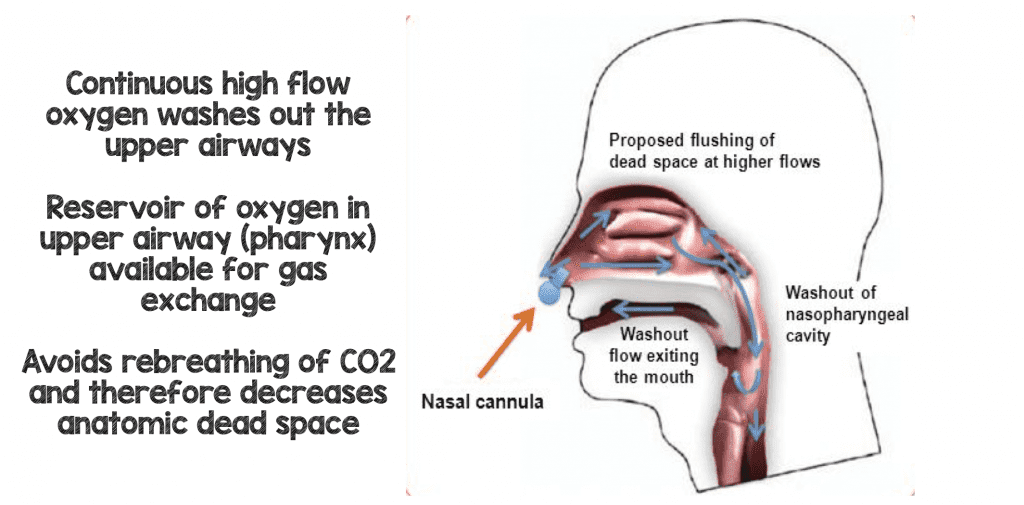
One of the major benefits of HFNC (some argue it’s actually the main benefit) is that it gives you a continuous flow of fresh gas at high flow rates replacing or washing out the patient’s pharyngeal dead-space (the old gas low in oxygen and high in CO2). Each breath that the patient now re-breathes will be washed out of carbon dioxide and replaced with oxygen rich gas improving breathing efficiency (8).
Guest Post Co-Written By
Frank Lodeserto, MD
AND:

Thomas Lettich, D.O.
Internal Medicine/Pediatrics Resident Physician
Geisinger Medical Center
Danville, Pennsylvania
References:
- Chidekel, A et al. The Effects of Gas Humidification with High-Flow Nasal Cannula on Cultured Human Airway Epithelial Cells. Pulmonary Medicine 2012. PMID: 22988501
- Dysart, K et al. Research in High Flow Therapy: Mechanisms of Action. Respiratory Medicine 2009. PMID: 19467849
- Katz, JA et al. Inspiratory Work with and Without Continuous Positive Airway Pressure in Patients with Acute Respiratory Failure. Anesthesiology 1985. PMID: 3904528
- Parke R et al. Pressures Delivered by Nasal High Flow Oxygen During all Phases of the Respiratory Cycle. Respiratory Care 2013. PMID: 23513246
- Frat JP et al. High-Flow Nasal Oxygen Therapy and Noninvasive Ventilation in the Management of Acute Hypoxemic Respiratory Failure. Annals of Translational Medicine 2017). PMID: 28828372
- Riera J et al. Effect of High-Flow Nasal Cannula and Body Position on End-Expiratory Lung Volume: A Cohort Study Using Electrical Impedance Tomography. Respiratory Medicine 2013. PMID: 23050520
- Roca O et al. Patients with New York Heart Association Class III Heart Failure may Benefit with High Flow Nasal Cannula Supportive Therapy: High Flow Nasal Cannula in Heart Failure. Journal Crit Care 2013. PMID: 23602035
- Möller W et al. Nasal High Flow Clears Anatomical Dead Space in Upper Airway Models. Journal of Applied Physiology 2015). PMID: 25882385
Support the Show by Paying & Claiming 0.5hrs of CME/CEH by Clicking on the Logo Below
Post Peer Reviewed By: Salim R. Rezaie, MD (Twitter: @srrezaie)
The post High Flow Nasal Cannula (HFNC) – Part 1: How It Works appeared first on REBEL EM - Emergency Medicine Blog.