
 Background: Ketamine’s role in the ED has expanded in recent years. The clinical reasons for this make it easy to understand why, and include analgesia, amnesia, and anesthesia. Amazingly, ketamine does not only reduce acute pain, but it also decreases persistent chronic and neuropathic pain as well. More importantly, use of low-dose ketamine (0.1 – 0.3 mg/kg IV) has been demonstrated to be opioid sparing. Some of the major issues with IV push low-dose ketamine include its adverse effects, such as feelings of unreality, nausea/vomiting, and dizziness. Many emergency medical providers have anecdotally noticed a decrease in adverse effects when ketamine is given slowly. In the paper we are reviewing today, the authors tried to see if increasing the duration of the ketamine from IV push (3 – 5 min) to a slow infusion (10 – 15 min) could mitigate some of these effects, while maintaining analgesic efficacy.
Background: Ketamine’s role in the ED has expanded in recent years. The clinical reasons for this make it easy to understand why, and include analgesia, amnesia, and anesthesia. Amazingly, ketamine does not only reduce acute pain, but it also decreases persistent chronic and neuropathic pain as well. More importantly, use of low-dose ketamine (0.1 – 0.3 mg/kg IV) has been demonstrated to be opioid sparing. Some of the major issues with IV push low-dose ketamine include its adverse effects, such as feelings of unreality, nausea/vomiting, and dizziness. Many emergency medical providers have anecdotally noticed a decrease in adverse effects when ketamine is given slowly. In the paper we are reviewing today, the authors tried to see if increasing the duration of the ketamine from IV push (3 – 5 min) to a slow infusion (10 – 15 min) could mitigate some of these effects, while maintaining analgesic efficacy.
What They Did:
- Randomized patients presenting to the ED with acute abdominal, flank, or musculoskeletal pain with an initial pain score of ≥5 to: Ketamine 0.3mg/kg by either IV Push (over 5min) or Short Infusion (0.3mg/kg mixed in 100mL normal saline solution over 15min) with Placebo Double-Dummy (both groups got an iv push, and an infusion).
Outcomes:
- Primary Outcome: Safety Efficacy at 5, 15, 30, 60, 90, and 120 min post administration
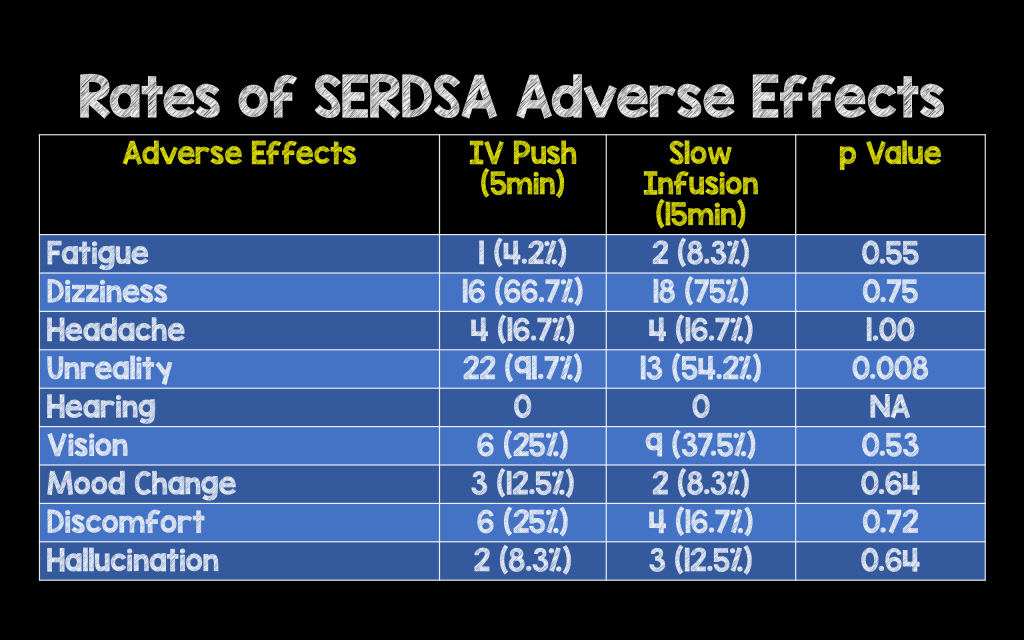
- Side Effects Rating Scale of Dissociative Anesthetics (SERSDA): Measures the severity of nine adverse effects with a score of 0 – 4 for each adverse effect. 0 = side effects absent and 4 = adverse effect is bothersome
- Richmond Agitation-Sedation Scale (RASS): A score of -4.0 – 4.0 with -4 = deeply sedated, 0 = alert and calm, and 4 = combative
- Secondary Outcomes:
- Analgesic Efficacy via Numerical Pain Rating Scale (NRS): A score of 0 – 10
- Changes in Vital Signs
- Need for Rescue Analgesia
Inclusion:
- Adults 18 – 65 years of age presenting to the ED
- Primary complaint for management of acute abdominal, flank, back, traumatic chest or musculoskeletal pain
- Intensity of pain ≥5 on the Numeric Pain Rating Scale
- Able to Consent
Exclusion:
- Pregnancy
- Breast Feeding
- Altered Mental Status
- Allergy to Ketamine
- Weight <46kg or >115kg
- Unstable vital signs (SBP <90 or >180mmHg, Pulse rate <50 or >150bpm, and RR <10 or >30 BPM)
- Medical history of acute head or eye injury
- Seizure
- Intracranial hypertension
- Renal or hepatic insufficiency
- Alcohol or drug abuse
- Psychiatric Illness
- Recent (4h before) analgesic use
Results:
- 48 patients enrolled in the study
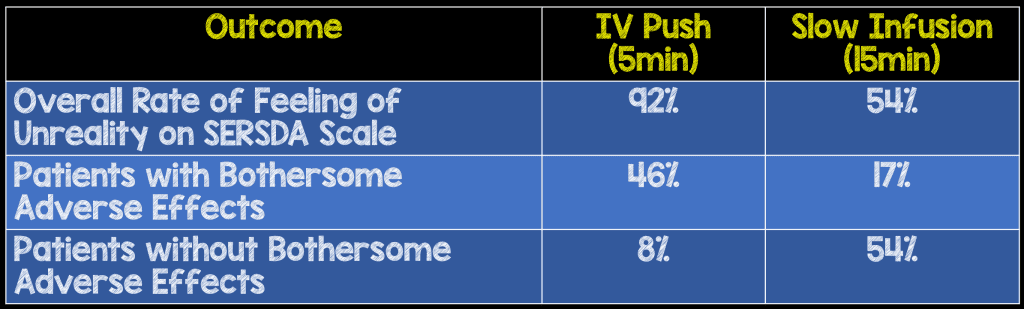
- Median Severity of Feeling of Unreality on SERDSA at 5 min
- IVP: 3.0
- SI: 0.0
- P=0.001
- Median RASS Scale at 5 min
- IVP -2.0
- SI: 0.0
- P = 0.01
- Decrease in Mean Pain Scores from Baseline to 15 min
- IVP: 5.2 +/- 3.53
- SI: 5.75 +/- 3.48
- No Statistical Differences with Respect to Changes in Vital Signs and Need for Rescue Medication
- There was no statistical difference on the SERSDA scale for 8 of the variables measured: headache, fatigue, dizziness, hearing, vision, mood change, discomfort, hallucination.
Strengths:
- Double dummy design: All participants received a corresponding placebo in order to keep patients and providers blinded
- Dummy IV push or Slow infusion given simultaneously to maintain blinding
- Treating providers, patients and the data collecting research team blinded to medication route received
- No difference in baseline pain
Limitations:
- Convenience Sample: Patients not enrolled consecutively (Only Monday – Friday 8a – 8p)
- Single center study
- Small sample size did not allow for assessment of variance in safety profiles of the two routes of administration (i.e. statistical significance) or for possible differences in the other SERSDA assessed adverse effects.
Discussion:
- If patients required additional pain medication 30 min after study drug administration, 0.1mg/kg IV morphine was offered as a rescue analgesic.
- Several studies have shown a correlation to side effects of low-dose ketamine with rapid rates of infusion. The pharmacologic reason for this is ketamine’s lipophilicity allows for rapid penetration of the blood-brain barrier and rapid saturation of the NMDA/glutamate receptors.
- Excluded head / eye injured patients despite ample evidence that ketamine is safe in these populations.
- The authors note that in their institution a 15 min infusion is billed the same as an IV push.
- One issue with slow infusion would be the availability of an infusion pump, however the authors discuss hanging the infusion, and running over approximately 15 min, without using an infusion pump. This saves time setting up the pump, and saves the issue of running out of pumps. We emailed the lead author Sergey Motov about this and his response was as follows:
“In my ED, we do not routinely use an IV infusion pump for a short infusion of SDK. After 6 years of doing so we have had no major adverse effects. Our nurses and ED pharmacists are very comfortable with a no pump approach by adjusting the flow rate to a 15 min time frame. Furthermore, we cap the max dose at 30 mg even if patient’s weight exceeds 100 kg which adds additional safety/comfort to our staff. This only applies to short infusion. For continuous drips we use IV infusion pumps. ”
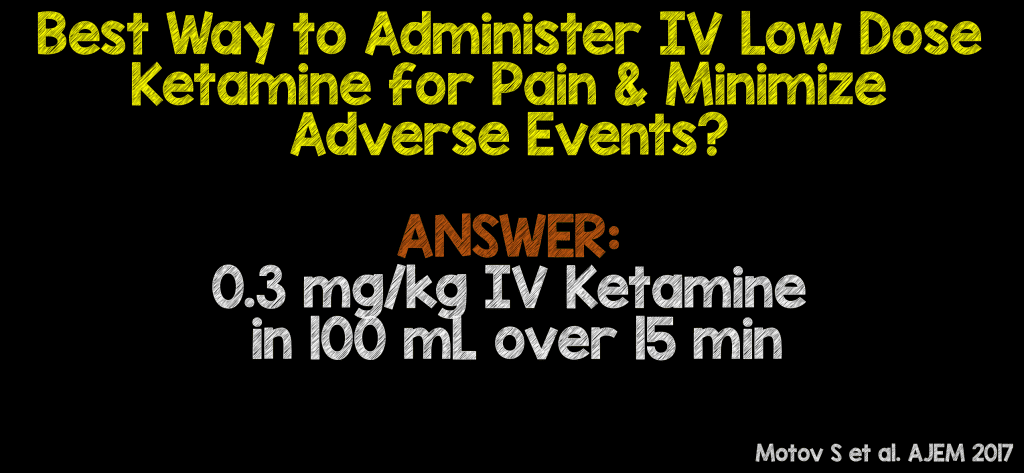
Author Conclusion: “Low-dose ketamine given as a short infusion is associated with significantly lower rates of feeling of unreality and sedation with no difference in analgesic efficacy in comparison to intravenous push.”
Clinical Take Home Point: Low dose ketamine of 0.3mg/kg, mixed into 100mL of Normal Saline given over slow infusion (15 minutes) has a decreased side effect (i.e hallucinations or dizziness) and equal analgesic profile when compared to IV push (5 minutes) low dose ketamine.
References:
- Motov S et al. A Prospective Randomized, Double-Dummy Trial Comparing Intravenous Push Dose of Low Dose Ketamine to Short Infusion of Low Dose Ketamine for Treatment of Moderate to Severe Pain in the Emergency Department. AJEM 2017; S0735 – 6757(17): 30171 – 7. PMID: 28283340
For More Thoughts on This Topic Checkout:
- Bryan Hayes at The PharmERToxGuy: How to Administer Low-Dose IV Ketamine for Pain in the ED
- Ken Milne at The SGEM: SGEM #198 – Better Slow Down – Push vs Short Infusion of Low Dose Ketamine for Pain in the Emergency Department
Post Peer Reviewed By: Rob Bryant (Twitter: RobJBryant13)
The post Low-Dose Ketamine for Acute Pain in the ED: IV Push vs Short Infusion? appeared first on REBEL EM - Emergency Medicine Blog.
