
 Background: Acute coronary syndrome (ACS) is a true spectrum of disease: STEMI, NSTEMI, Unstable Angina (UA), and Stable Angina (SA). The history and physical plus ECG help us to differentiate patients with STEMI from NSTEMI. Classically, STEMI represents complete occlusion of a culprit artery and this finding requires immediate coronary angiography and revascularization. It turns out that there is a subset of NSTEMI patients that also have complete total occlusion (TO) of culprit arteries despite not having true ST elevation on ECG, which unfortunately causes delays in definitive treatment.
Background: Acute coronary syndrome (ACS) is a true spectrum of disease: STEMI, NSTEMI, Unstable Angina (UA), and Stable Angina (SA). The history and physical plus ECG help us to differentiate patients with STEMI from NSTEMI. Classically, STEMI represents complete occlusion of a culprit artery and this finding requires immediate coronary angiography and revascularization. It turns out that there is a subset of NSTEMI patients that also have complete total occlusion (TO) of culprit arteries despite not having true ST elevation on ECG, which unfortunately causes delays in definitive treatment.
What They Did:
- Meta-analysis to estimate the difference in outcomes between totally occluded and non-totally occluded culprit arteries in patients with NSTEMI
Outcomes:
- Major Cardiac Adverse Events (MACE): Death, non-fatal MI, or target vessel revascularization
- All-Cause Mortality
Definitions:
- Short-Term = In- Hospital or 30-Day
- Medium to Long-Term = 6 – 12 months
Results:
- 7 studies with 40,777 patients
- 25.5% (10,415 patients) had a completely occluded culprit artery with a predominant infero-lateral distribution (40% right coronary and 33% left circumflex artery)
- 74.5% (30,362 patients) had non-completely occluded culprit artery
- Anatomical Distribution of Culprit Arteries
- Right Coronary Artery: TO 40% vs non-TO 28%
- Left Circumflex Artery: TO 32% vs non-TO 28%
- Left Anterior Descending Artery: TO 28% vs non-TO 44%
- Time to Angiography
- TO: 31.3hr vs non-TO 34.2hr
- Increased Risk of MACE in the short-term with TO of culprit artery: RR 1.41; CI 1.17 – 1.70, p = 0.0003
- Increased Risk of MACE in the medium to long-term with TO of culprit artery: RR 1.32; CI 1.11 – 1.56, p = 0.001
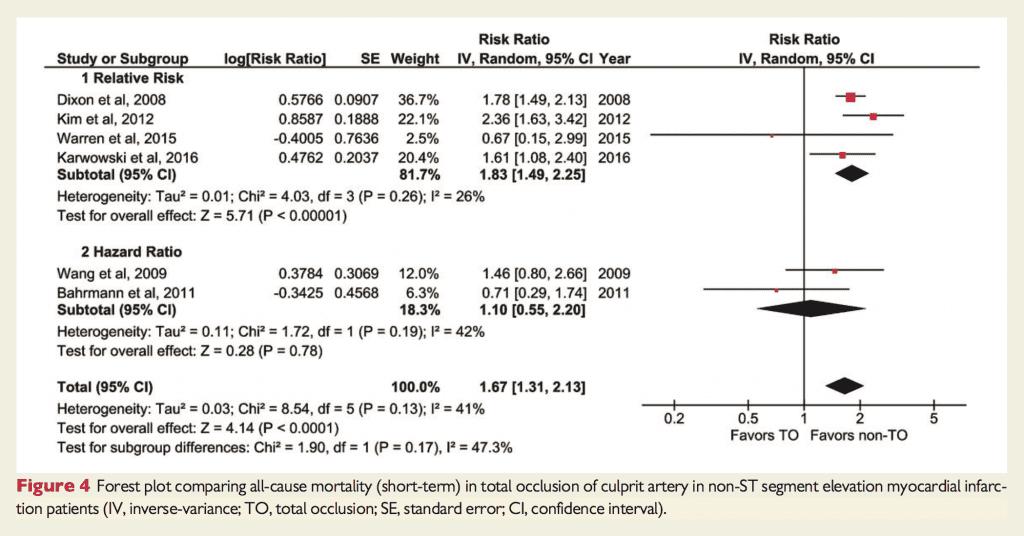
- Increased short term mortality with TO of the culprit artery: RR 1.67; CI 1.31 – 2.13, p <0.0001
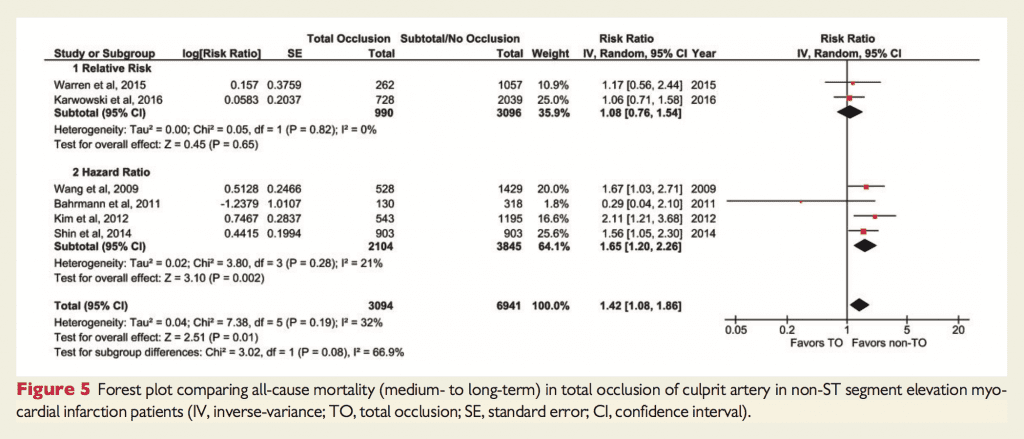
- Increased Risk of medium to long-term mortality with TO of the culprit artery: RR 1.42; 1.08 – 1.86, p = 0.01
Strengths:
- Followed PRISMA guidelines for this review
- Assessed the quality of studies included in the review using the Grading of Recommendations, Assessment, Development and Evaluation (GRADE)
- Studies included had good methodological quality
- Culprit artery identified via gold standard (angiographic findings)
- No difference in rates of revascularization between groups that may bias results
Limitations:
- No RCTs in this review; All studies included were observational in nature (overall quality of evidence low due to risk of bias from observational design of included studies)
- Evidence affected by presence of between-study heterogeneity
- Sampling bias: Many NSTEMIs don’t get heart catheterization. The rate of total occlusion as well as the bad outcomes are likely exaggerated by the selection issues
Discussion:
- Although there was more MACE and all-cause mortality with total occlusion of culprit artery, there was no significant difference in high risk clinical features (i.e. There were no clinical features that were more likely to represent patients with TO)
- Due to the different assays of troponin used, results could not be pooled, however in reviewing the data total occlusion of culprit artery was more likely to cause more myocardial injury, and thus higher troponin levels relatively to non-total occlusion of culprit artery
- Explanations of Why There is an Absence of Characteristic ECG Changes:
- ECG has decreased sensitivity to show changes of TO in the infero-lateral distribution
- ST-elevation may be missed by routine ECG monitoring as coronary occlusion is a dynamic process
- Slow developing occlusive thrombus along with adequate collateral flow leading to only sub endocardial ischemia
Author Conclusion: “Our meta-analysis suggests that patients with NSTEMI who demonstrate a totally occluded culprit vessel on coronary angiography are at higher risk of mortality and major adverse cardiac events. Better risk stratification tools are needed to identify such high-risk acute coronary syndrome patients to facilitate earlier revascularization and potentially to improve outcomes.”
Clinical Take Home Point:
Total occlusion of culprit artery in acute NSTEMI have an increased risk of MACE and all-cause mortality compared to non-total occlusion, but unfortunately there are no significant differences in high risk clinical features that can allow us to stratify these patients. If you have a patient with NSTEMI and hemodynamic instability or features of ongoing ischemia, be an advocate for your patient and push for an early invasive strategy.
References:
- Khan AR et al. Impact of Total Occlusion of Culprit Artery in Acute Non-ST Elevation Myocardial Infarction: A Systematic Review and Meta-Analysis. Eur Heart J 2017. PMID: 29020244
Post Peer Reviewed By: Anand Swaminathan (Twitter: @EMSwami)
The post NSTEMIs Are Not All the Same appeared first on REBEL EM - Emergency Medicine Blog.
