
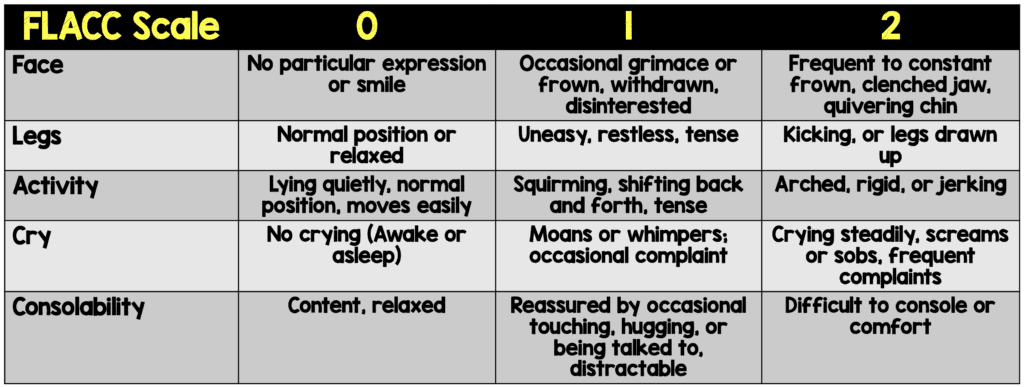
 Background: Oral sweet solutions have been used for some time as a pain-reducing agent for procedures in the neonatal population. However, there has been some mixed results in its effectiveness, especially in the <12 months of age group. Nasopharyngeal aspiration (NPA) is a common procedure performed especially during seasonal upper respiratory tract infection. A study performed in 2005 by Macfarlane et al [2], demonstrated that NPA had a Face, Legs, Activity, Cry, and Consolability pain scale (FLACC) score of 6 out of 10.
Background: Oral sweet solutions have been used for some time as a pain-reducing agent for procedures in the neonatal population. However, there has been some mixed results in its effectiveness, especially in the <12 months of age group. Nasopharyngeal aspiration (NPA) is a common procedure performed especially during seasonal upper respiratory tract infection. A study performed in 2005 by Macfarlane et al [2], demonstrated that NPA had a Face, Legs, Activity, Cry, and Consolability pain scale (FLACC) score of 6 out of 10.
Paper: Gouin S et al. Effect on Pain of an Oral Sucrose Solution vs. Placebo in Children 1 to 3 Months Old Needing Nasopharyngeal Aspiration: A Randomized Controlled Trial. JEM 2021. PMID: 33795167
Clinical Question: Does oral sucrose solution alleviate pain in children (1 to 3 months of age) during nasopharyngeal aspiration (NPA) compared to placebo?
What They Did:
- Randomized, double-blind, placebo-controlled clinical trial at a single pediatric ED
- NPA = Removal of nasopharyngeal secretions using a catheter (6 or 8 French) inserted into each nostril, one after the other
- 2 minutes prior to procedure randomized to:
- Sucrose: 2mL of 88% sucrose
- Placebo: 2mL of placebo
Outcomes:
- Primary: Mean difference in pains scores at 1 min post NPA assessed by Face, Legs, Activity, Cry, and Consolability (FLACC) Pain Scale
-
Secondary:
- Difference between both groups for:
- Neonatal Infant Pain Scale (NIPS)
- Crying tine
- Heart rate
- Side effects and adverse events
- Difference between both groups for:
FLACC Score:
Inclusion:
- 1 to 3 months of age
- Requiring NPA
Exclusion:
- Infants born prematurely
- Infants with chronic oropharyngeal malformations or dysfunction (i.e. cleft palate or micrognathia)
- Severe respiratory distress (Respiratory Distress Assessment of Illness score >10
- Assisted ventilation (ie. tracheostomy or oxygen dependency)
- Previous participation in the study
- Painful procedures in the preceding 60min (bladder catheterization, bladder puncture, lumbar puncture, capillary blood tests)
- Parental language barrier (not able to speak French or English)
Results:
- 99 patients were eligible
- 11 missed, 3 excluded due to exclusion criteria, and 9 families refused to participate
- 76 patients were randomized but 4 patients had protocol deviations and excluded
- 72 patients completed the trial
-
Mean Difference in FLACC Scores Compared with Baseline at 1 Minute (Primary Outcome):
- Sucrose: 3.3 (2.5 to 4.1)
- Placebo: 3.2 (2.3 to 4.1)
- P = 0.094
- Mean Difference in FLACC Scores Compared with Baseline at 3 Minutes:
- Sucrose: -1.2 (-.17 to 0.7)
- Placebo -0.8 (-1.5 to -0.1)
- P = 0.66
- Mean Difference in Neonatal Infant Pain Scale Scores at 1 Minute:
- Sucrose: 2.3 (1.6 to 3.0)
- Placebo: 2.5 (1.8 to 3.2)
- P = 0.086
- Mean Difference in Neonatal Infant Pain Scale Scores at 3 Minutes:
- Sucrose: -1.2 (-1.6 to -0.8)
- Placebo: -0.8 (-1.3 to 0.2)
- P = 0.59
- Difference in Mean Crying Time:
- Sucrose: 114s (98 to 130)
- Placebo 109s (92 to 126)
- P = 0.81
- Heart Rate at 1 Minute:
- Sucrose: 174BPM (154 to 194)
- Placebo: 179BPM (160 to 198)
- P = 0.32
Strengths:
- Placebo similar in color and packaging as oral sucrose solution to maintain blinding
- Pharmacist supervising randomization not involved in the study. Therefore, all providers involved in patient’s care and patients were blinded to group assignment until data analysis completed
- Demographic characteristics, baseline FLACC scores, baseline NIPS scale, and heart rates of the two groups were similar
- Used well validated pain scales including FLACC, NIPS, and crying time
Limitations:
- Convenience sample as patients only enrolled between 8am to 6pm on weekdays when research nurses were available
- Small number of participants not allowing for sub analyses. Additionally, confidence intervals are rather wide due to the small numbers of patients
- Pain in the 0 – 3-month age group is based on observation of the patient and not self-reports which is rather subjective
- Pain scores were not measured during the procedure. This misses the most painful aspect of the procedure, which most likely underestimates the amount of pain felt by infants
- NPA may not be painful, but more distressing, however this is hard to distinguish in neonates that cannot self-report
- Blinded but, physician/parent may have been unblinded by smell or stickiness of solution
- Length of aspiration was longer in placebo group by 24 seconds. Placebo may actually be better than what is seen in this study. Unclear why suctioning in the placebo group was different/longer
- No inter-rater reliability for FLACC score
Discussion:
- There was no statistically significant decrease in pain score assessed by FLACC and NIPS scales, or crying time while using sucrose compared to placebo in NPA among infants aged 1 to 3 months of age in this trial
- These results are in line with previous randomized clinical trials about the ineffectiveness of oral sucrose for pain reduction in infants:
- Gouin et al [3] failed to demonstrate reductions in pain score, vital signs and crying time in infants 1 – 3 months of age getting simple venipuncture
- Desjardins et al [4] failed to demonstrate a decrease in pain score during IV cannulations
- Rogers et al [5] also showed no reduction in pain for infants ≤90 days old getting bladder catheterization
- Is NPA really a painful procedure? In the intro the authors note a prior study showing a FLACC of 6 with NPA, but in this study the max FLACC score was only in the 4.5 range. Perhaps using sucrose solution didn’t matter because NPA simply wasn’t that painful in the way it was performed in this study
Author Conclusion: “In infants (1 – 3 months) undergoing NPA, administration of an oral sweet solution did not statistically decrease pain scores.”
Clinical Take Home Point: This trial, along with previous RCTs highlight an important point that oral sucrose may not be a valid option in pain management among young infants. There is a need to identify better strategies to improve pain management in this unique patient population.
References:
- Gouin S et al. Effect on Pain of an Oral Sucrose Solution vs. Placebo in Children 1 to 3 Months Old Needing Nasopharyngeal Aspiration: A Randomized Controlled Trial. JEM 2021. PMID: 33795167
- Macfarlane P et al. RSV Testing in Bronchiolitis: Which Nasal Sampling Method is Best? Arch Dis Child 2005. PMID: 15908632
- Gouin S et al. A Randomized Double-Blind Trial Comparing the Effect on Pain of an Oral Sucrose Solution vs. Placebo in Children 1 to 3 Months Old Undergoing Simple Venipuncture. JEM 2018. PMID: 29108736
- Desjardins MP et al. A Randomized Controlled Trial Evaluating the Efficacy of Oral Sucrose in Infants 1 to 3 Months Old Needing Intravenous Cannulation. Acad Emerg Med 2016. PMID: 27098499
- Rogers AJ et al. A Randomized, Controlled Trial of Sucrose Analgesia in Infants Younger than 90 Days of Age who Require Bladder Catheterization in the Pediatric Emergency Department. Acad Emerg Med 2006. PMID: 16636358
For More Thoughts on This Topic Checkout:
- First10EM: Sucrose is Not a Pain Medication
Post Peer Reviewed By: Anand Swaminathan, MD (Twitter: @EMSwami)
The post Oral Sucrose for Pain Control in Infants: A Useless Practice? appeared first on REBEL EM - Emergency Medicine Blog.
