 Background: The clinical diagnosis of pulmonary embolism (PE) can be challenging given its variable presentation, thus requiring dependence on objective testing. decision instruments such as PERC and the Wells’ score help stratify patients to low or high probability, enabling focused use of CT pulmonary angiography (CTPA) for diagnosis. However, despite these algorithms, there is evidence of increasing use of CTPA along with diminishing diagnostic rates (less than 10%). This combination results in the overdiagnosis of subsegmental PEs, unnecessary exposure to radiation and false positive results.
Background: The clinical diagnosis of pulmonary embolism (PE) can be challenging given its variable presentation, thus requiring dependence on objective testing. decision instruments such as PERC and the Wells’ score help stratify patients to low or high probability, enabling focused use of CT pulmonary angiography (CTPA) for diagnosis. However, despite these algorithms, there is evidence of increasing use of CTPA along with diminishing diagnostic rates (less than 10%). This combination results in the overdiagnosis of subsegmental PEs, unnecessary exposure to radiation and false positive results.
Though the D-dimer test has long been maligned for its low specificity the real issues around it rest in indiscriminate use and threshold value. In recent years, age-adjustment of the D-dimer and the YEARS algorithm have attempted to adjust the threshold in order to “rule-out” more patients without advanced imaging. The YEARS creates a two-tiered D-dimer threshold by first asking three questions:
- Are there clinical signs of DVT?
- Does the patient have hemoptysis? and
- Is PE the most likely diagnosis.
If the answer to all 3 questions is no, the D-dimer threshold is set at 1000 ng/mL FEU (500 ng/mL DDU) and if the answer is “yes” to any of the 3 questions, the D-dimer threshold is set at 500 ng/mL FEU (250 ng/mL DDU). More recently, the YEARS algorithm has been assessed in pregnancy.
Age-adjustment of the D-dimer assay simply multiplies 10 X the patients age (if using FEU and 5 X age if using DDU) and uses this number as the threshold for the test. This adjustment is applied to patients > 50 years of age. Age-adjustment of the D-dimer was endorsed by an ACEP clinical policy in 2018.
The PEGeD study is another attempt to show the safety of using an adjusted D-dimer threshold.
From Research to Practice Episoe 2.0 – The PEGeD Trial
[embedyt] https://www.youtube.com/watch?v=pxxRNpUsPak[/embedyt]
Also Be Sure to Checkout our YouTube Channel

Article: Kearon C et al. Diagnosis of Pulmonary Embolism with D-dimer Adjusted to Clinical Probability. NEJM 2019; 381(22): 2125-34. PMID: 31774957
Clinical Question: Does a probability based D-dimer threshold safely exclude the diagnosis of PE without further imaging?
Population: Outpatients (Emergency Department patients or outpatient clinics) > 18 years of age with symptoms or signs suggestive of PE.
Study Protocol:
- Eligible patients were assessed for PE risk using the seven-item Wells clinical prediction rule to categorize patient’s clinical pre-test probability (C-PTP) as low (Wells 0-4.0), moderate (4.5 – 6.0) or high (> 6.5)
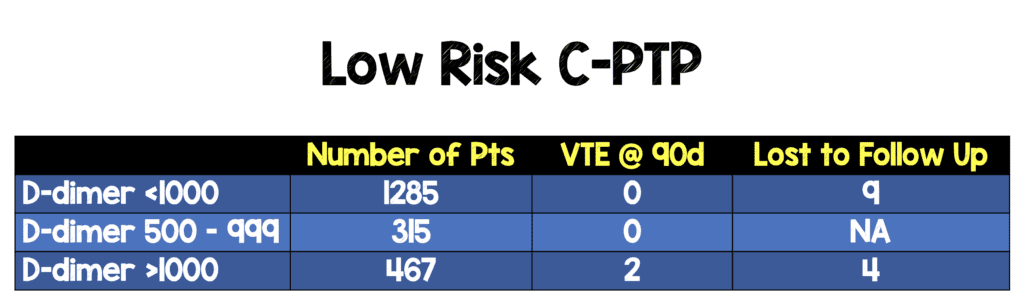
- D-dimer threshold set to 1000 ng/ml FEU for low C-PTP
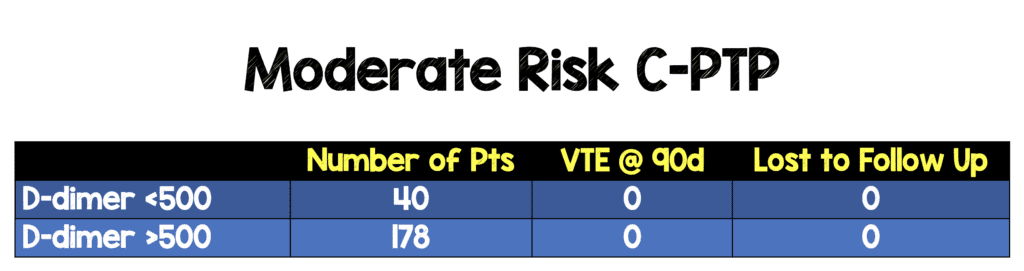
- D-dimer threshold set to 500 ng/ml FEU for moderate C-PTP (standard workup is to use only high-sensitivity D-dimer to rule out in moderate risk group)
- High C-PTP patients went directly to chest imaging without D-dimer testing
- Patients who were below the D-dimer threshold were discharged without chest imaging
Outcomes:
- Primary: Incidence of VTE during 90-day follow-up period among patients with low or moderate C-PTP and negative D-dimer testing who did not receive AC therapy
-
Secondary:
- Percentage of patients with VTE in predefined subgroups
- Bleeding events and deaths
- Percentage of patients who avoided undergoing chest imaging because they had low C-PTP and D-dimer of 500-999 ng/ml FEU or moderate C-PTP and D-dimer < 500 ng/ml FEU
Design: Prospective study in university-based clinical centers in Canada
Excluded:
- < 18 years of age
- Received full-dose anticoagulation (AC) for > 24 hours
- Major surgery < 21 days
- D-dimer level known prior to C-PTP assessment
- Chest imaging performed contrary to protocol
- Undergone contrast-enhanced CT of the chest for another reason
- Ongoing need for AC
- Life expectancy < 3 months
- Pregnant
- Geographically inaccessible for follow-up
Primary Results:
-
- Patients assessed: 3133
-
Patients registered (after exclusions applied): 2056
- An additional 39 patients were excluded after initially being thought to meet eligibility criteria
- Final enrollment: 2017
- PE diagnosed in 7.4% of patients enrolled in the study
-
C-PTP Assessment
- Low C-PTP: 1752
- Moderate C-PTP: 218
- High C-PTP: 47
Critical Findings:
-
High C-PTP
- n = 47
- PE on Initial Imaging: 19/28
- Lost to follow up = 0
- VTE at 90 days: 0/28
- Overall, 0 out of 1325 patients who were negative by adjusted threshold D-dimer in the low and moderate C-PTP group had a VTE at 90 days
Strengths:
- Examines an important clinical question in an attempt to decrease imaging in the assessment of pulmonary embolism
- Multicenter study with reasonable and limited exclusions increasing applicability
- Follow up at 90 days was excellent (< 5% lost to follow up)
- Reported subgroups were predefined
- Study was not industry supported
Limitations:
- Unclear how many patients overall would be eligible in the clinical settings that were investigated. This data set may represent a convenience sample
- Overall, healthy group of patients with only 13% of patients were moderate or high C-PTP
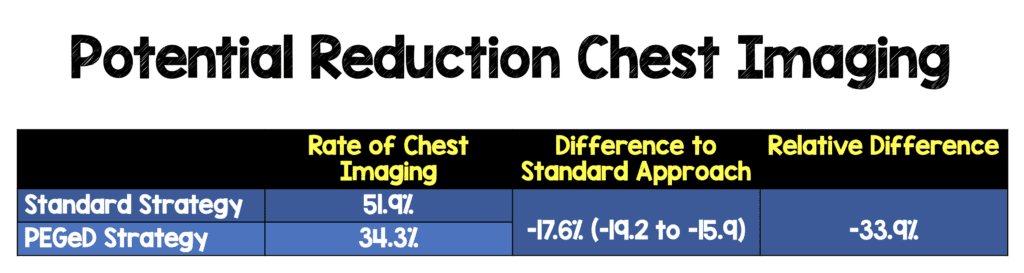
- PEGeD approach not directly compared to standard approach (compared theoretically)
- Cannot apply results to pregnant patients as this group was excluded from enrollment
- Some of the exclusion criteria were subjective (I.e. life expectancy < 3 months, geographically inaccessible to follow up)
Discussion:
-
Enrolled patients may represent a convenience sample
- The authors are unsure of how many patients were screened and not further assessed
- Possibility that patients at very low risk were selectively recruited making performance of PEGeD approach look better than it actually is
-
Overall, the enrolled patients were not very sick (only 13% non-low risk and only 2% high-risk)
- Data on using D-dimer in moderate risk group inconclusive due to low number of patients in this cohort
- This is much more of a study of application of a higher D-dimer threshold in low C-PTP patients
- PEGeD approach not directly compared in this study to standard approach. The comparison to standard is hypothetical but, may not represent contemporaneous practice
- This approach seems very similar to the YEARS protocol but, there is an important difference. Clinicians may have assessed PE to be the most likely diagnosis and still include them in the adjusted D-dimer threshold as having only this variable of the Wells would still result in a low C-PTP.
- Very few patients were lost to follow up. However, if we assume that all patients lost to follow up developed a VTE in the 90 day period, this would give a rate of 0.15% VTE at 90 day follow up.
-
There were only 2 VTEs diagnosed at 90 days, both in the low C-PTP cohort
- One had D-dimer > 1000, negative index CTPA and found to have a DVT on follow up
- One had D-dimer > 1000, positive CTPA and found to have another acute PE on follow up
- Primary outcome looked at VTE at 90 days. Is this as important as finding PE at 90 days? Missing a DVT is not as concerning to me as missing a PE.
Authors Conclusions:
“A combination of a low C-PTP and a d-dimer level of less than 1000 ng per milliliter identified a group of patients at low risk for pulmonary embolism during follow-up.”
Our Conclusions:
We agree with the authors. In a group of low pre-test probability patients for pulmonary embolism based on a Wells < 4, the D-dimer threshold can be safely set to 1000 ng/ml FEU (500 ng/ml DDU).
Potential to Impact Current Practice: Using the PEGeD approach, much like using YEARS or age-adjusted D-dimer approaches, can safely reduce the use of imaging in the evaluation of pulmonary embolism.
Bottom Line: The use of variable D-dimer thresholds based on clinical pre-test probability in the assessment of pulmonary embolism can reduce chest imaging and is ready for widespread ED use.
For More on This Topic Checkout:
- St. Emlyn’s: Level Pegging? JC and the PEGeD Study
- EM Lit of Note: YEARS, But Wells
- REBEL EM: The YEARS Study – Simplified Diagnostic Approach to PE
- REBEL EM: Age Adjusted D-dimer Testing
- REBEL EM: ACEP Clinical Policy on Acute VTE 2018
- The Bottom Line: PEG-eD
- JournalFeed: Is it Time to Adjust D-Dimer Thresholds to Our Clinical Pretest Probability?
- The SGEM: SGEM #282 – It’s All ‘Bout That Bayes, ‘Bout That Bayes – No Trouble – In Diagnosing Pulmonary Embolism
Post Peer Reviewed By: Salim R. Rezaie, MD (Twitter: @srrezaie)
The post PEGeD Study – Is It Safe to Adjust the D-Dimer Threshold for Clinical Probability? appeared first on REBEL EM - Emergency Medicine Blog.