
 Definition: Blood loss > 500 ml after a delivery (or > 250 ml after an abortion). The management of post-abortion hemorrhage is similar to that of post-partum hemorrhage (PPH).
Definition: Blood loss > 500 ml after a delivery (or > 250 ml after an abortion). The management of post-abortion hemorrhage is similar to that of post-partum hemorrhage (PPH).
Definition ADDENDUM: 03/04/2021
ACOG Updated Definition: “is defined as cumulative blood loss of greater than or equal to 1,000mL or blood loss accompanied by signs or symptoms of hypovolemia within 24 hours.” [Link is HERE]
Causes
- Uterine atony (~ 50% of cases)
- Retained products of conception (POCs)
- Cervical lacerations
- Uterine perforation
- Uterine Inversion
- Abnormal placentation (accreta, increta, percreta)
- Coagulopathy
Background:
- Occurs in 1-2% of patients undergoing a first trimester surgical abortion
- Most common cause of abortion-related mortally in 2nd trimester
- Risk increases with increasing maternal age
Clinical Presentation
-
Diagnosis
- No exact definition but generally thought to be present when bleeding exceeds 500 ml
- Should be suspected if bleeding “exceeds a clinician’s estimate of ‘normal’.” (Lew 2013)
- Blood loss is not always brisk. Can be moderate, prolonged bleeding
- Tachycardia and hypotension will be late findings
- Look for signs of hypoperfusion
-
Key Examination Pieces
- Any abnormal vital signs should raise suspicion of PPH
- Obtain history for bleeding disorders or anticoagulation use
-
Examination of placenta
- Should be intact without “missing pieces”
- Looking for retained products of conception as source of ongoing bleeding
-
Examination of fundus of uterus
- Uterine atony (uterine muscles do not fully contract) is the most common cause of postpartum hemorrhage (~ 80% of cases) (Lew 2013)
- Abdominal examination will reveal a “boggy” uterus. Can be confirmed on bimanual exam
-
Direct examination of vagina
- Lacerations to genital tract during delivery can cause brisk blood loss
- Examine for uterine inversion (displacement of uterus into vagina)
-
Examine sites where blood drawn/IVs started
- Looking for oozing or ongoing bleeding that may signal the presence of disseminated intravascular coagulation (DIC)
Treatment
-
Basic Supportive Care
- Large bore IV X 2, supplemental O2 if hypoxic, cardiac monitor
-
Volume expansion to replace hemorrhage
- Replace with blood products as soon as available
- Give O negative until type specific products available
- Can use crystalloid early if evidence of hypoperfusion but not ideal resuscitative fluid
- Call obstetrics or surgical consultants early as patients frequently require surgical intervention
-
Fundal Massage (Robert’s + Hedges) Tranexamic Acid (TXA)
- Largest study to date demonstrated reduction in death due to hemorrhage (1.9% vs 1.5%) without difference in hysterectomy rate (WOMAN trial 2017)
-
Dose
- 1 gram over 10 minutes
- Second dose given if continued bleeding after 30 minutes or recurrent bleeding within 24 hours
- Full review of WOMAN trial found here
-
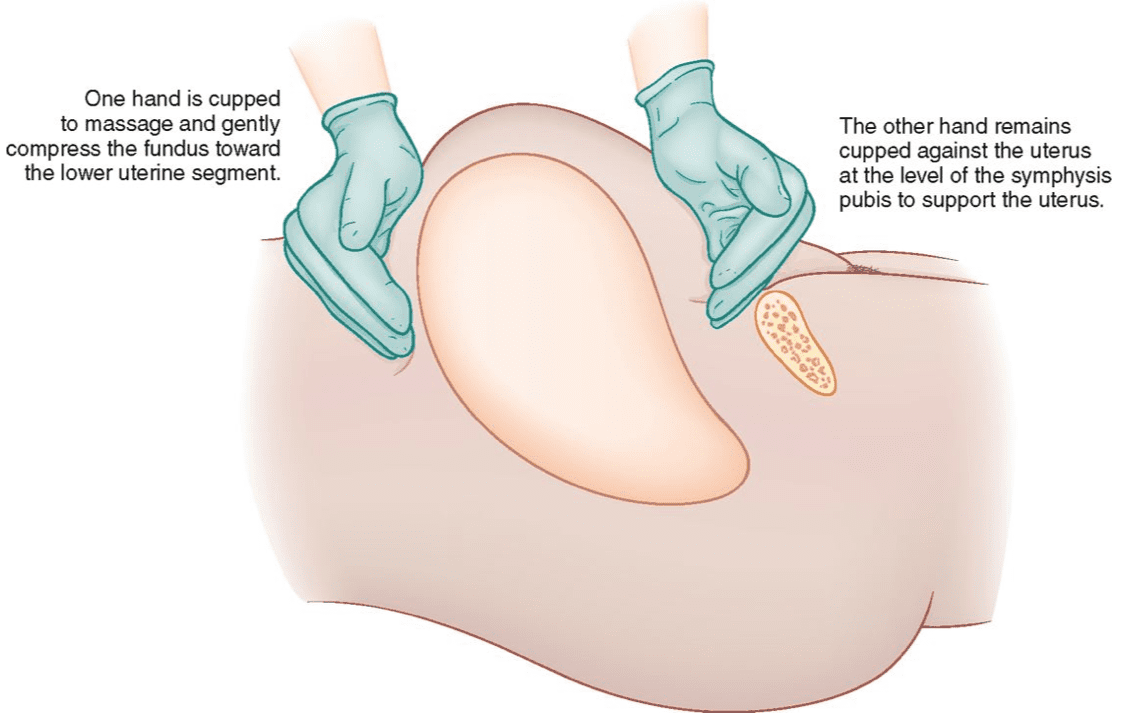
Uterine Massage
- First line treatment for uterine atony
- Begin with firm massage of the uterine fundus through the abdominal wall
-

Bimanual Uterine Massage (Robert’s + Hedges) Advance to bimanual uterine compression if bleeding continues
- External hand compresses and massages uterus
- Hand placed internally in fist to massage anterior aspect of uterus
- Avoid downward massage with internal hand (can cause uterine inversion or injure blood vessels)
-
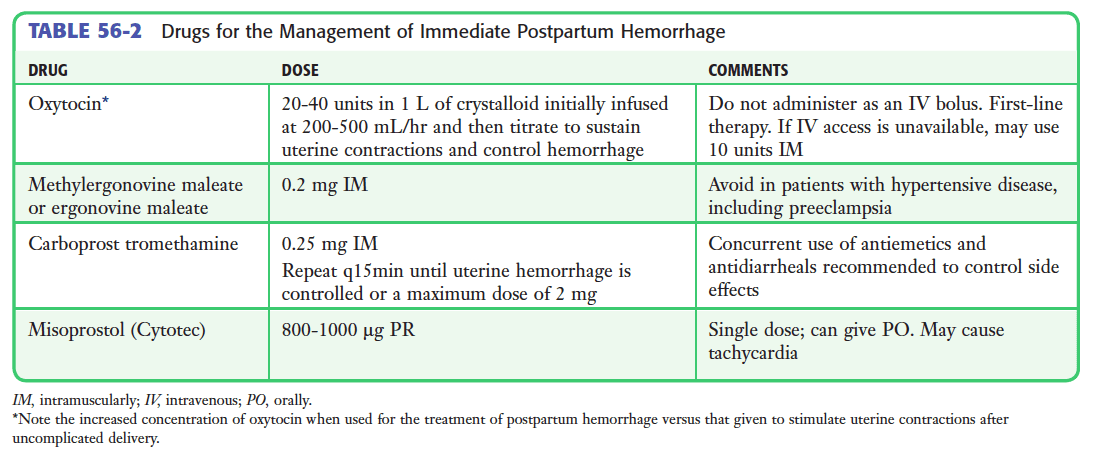
Uterotonic Medications
- Should be given concomitantly with uterine massage
- Multiple medication options which increase uterine muscle tone
-
Direct Uterine tamponade
- Uterine packing: Uterus is packed with gauze or hemostatic dressings
-
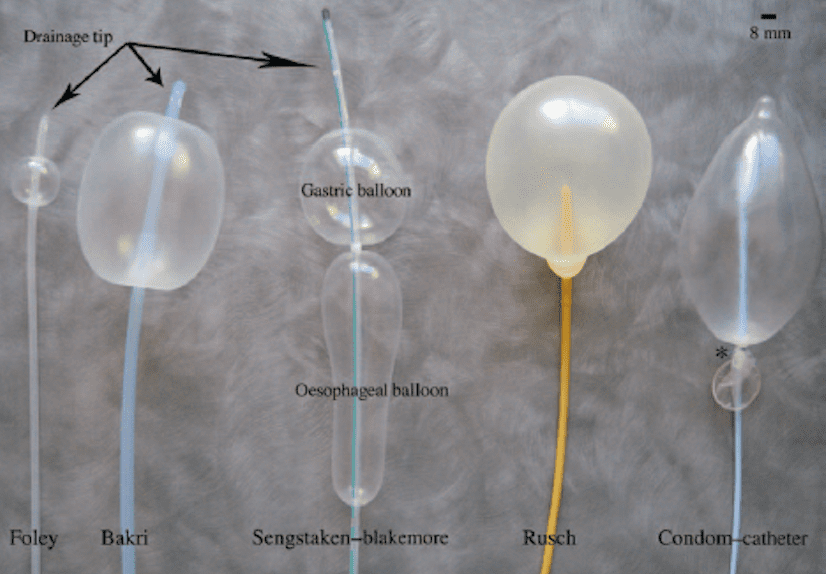
Balloon tamponade
- Device is placed into the uterus and balloon filled with saline or water
-

Bakri Balloon Bakri Balloon
- Commercially available device specifically for this indication
- Balloon accommodates up to 800 ml but as little as 250-500 ml of inflation can stop bleeding
- Can potentially obviate need for surgical management
-
Sengstaken-Blakemore Esophogastric tube
- Has a maximum volume ~ 500 ml
-
Latex Condom (Georgiou 2009, Burke 2017)
- Case reports + case series of condom secured to foley catheter and inflated
- Volume: 250-300 ml
-
Do not use a single foley catheter for this indication
- Balloon with only 80 ml volume at maximum
- More likely to hide bleeding than to tamponade it
- Case reports of placement of multiple foley catheters (Georgiou 2009)
-
Uterine Inversion
- Treatment involves reduction of the uterus back into position
- Typically requires procedural sedation or general anesthesia to accomplish
- Reduction can be facilitated with tocolytic agents (I.e. terbutaline or magnesium sulfate)
-
Disseminated Intravascular Coagulation
- Administer blood products and adjuncts based on clotting derangements that are present (See LITFL DIC Post)
- Patients will often require hysterectomy to resolve DIC
Take Home Points
- Watch for continued bleeding in excess of 500 ml or bleeding that is “more than normal.” Call it postpartum hemorrhage and start resuscitation
- Call your obstetric and/or surgical consultants early as operative intervention is often required
- Replace intravascular volume with blood products
- Uterine atony is the most common cause of postpartum hemorrhage. Begin treatment with uterine massage and uterotonic medications
- Consider the development in DIC when patients continue to bleed despite appropriate management
For More on This Topic Checkout:
- Core EM: Episode 33.0 – Post-Partum Hemorrhage
- Core EM: TXA in Post-Partum Hemorrhage
- LITFL: Disseminated Intravascular Coagulation
- emDocs: EM@3AM – Disseminated Intravascular Coagulation
References:
- Lew GH, Pulia MS: Emergency Childbirth, in Roberts JR, Hedges JR, Custalow CB, et al (eds): Clinical Procedures in Emergency Medicine, ed 6. Philadelphia, Saunders, 2013, Ch 56:p 1155-82.
- WOMAN Trial Collaborators. Effect of early tranexamic acid administration on mortality, hysterectomy, and other morbidities in women with postpartum hemorrhage (WOMAN): an international, randomised, double-blind, placebo-controlled trial. Lancet 2017; 389(10084): 2105-16. PMID: 28456509
- Georgiou C. Balloon tamponade in the management of postpartum haemorrhage: a review. BJOG 2009; 116(6): 748-57. PMID: 19432563
- Burke TF et al. Shock progression and survival after use of a condom uterine balloon tamponade package in women with uncontrolled postpartum hemorrhage. Int J Gynaecol Obstet 2017; 139(1): 34-8. PMID: 28675419
Post Peer Reviewed By: Salim R. Rezaie (Twitter: @srrezaie)
The post Post-Partum Hemorrhage appeared first on REBEL EM - Emergency Medicine Blog.
