
 Background/Introduction: Emergency department management of severe psychomotor agitation presents a unique challenge due to the undifferentiated nature of patient presentations, need for situational awareness, necessity for rapid sedation, all while ensuring safety and efficacy. Commonly used agents include a combination of benzodiazepines and antipsychotic medications for chemical sedation, but these have their own risks and inconsistent effectiveness. An ideal agent would allow for easy and fast administration without the need for intravenous access, have a rapid onset of action, and possess a wide therapeutic window with a favorable side effect profile.
Background/Introduction: Emergency department management of severe psychomotor agitation presents a unique challenge due to the undifferentiated nature of patient presentations, need for situational awareness, necessity for rapid sedation, all while ensuring safety and efficacy. Commonly used agents include a combination of benzodiazepines and antipsychotic medications for chemical sedation, but these have their own risks and inconsistent effectiveness. An ideal agent would allow for easy and fast administration without the need for intravenous access, have a rapid onset of action, and possess a wide therapeutic window with a favorable side effect profile.
This has led to the increase in the use of Ketamine for severe psychomotor agitation in the emergency department. It is able to be administered in multiple forms, including intramuscularly, crosses the blood-brain barrier with a rapid onset of action, has a favorable hemodynamic and side effect profile. Despite this, Ketamine still suffers from a lack of robust, prospective randomized controlled studies and variable adoption of this medication by the different emergency medicine and anesthesia societies.
Paper: Barbic D et al. Rapid Agitation Control With Ketamine in the Emergency Department: A Blinded, Randomized Controlled Trial. Ann Emerg Med. 2021. PMID: 34353650
Clinical Question: Does ketamine 5mg/kg IM or midazolam 5mg plus haloperidol 5mg IM result in more rapid sedation of acutely agitated patients in the ED?
What They Did:
- Randomized parallel-arm 1:1 clinical trial in a single center ED in Canada
- Patients randomized to:
- Intramuscular Ketamine: 5 mg/kg
- Intramuscular Midazolam and Haloperidol: 5 mg each
- RASS scores were documented at 5-minute intervals until either primary endpoint or 30-minutes elapsed.
- Adverse events were recorded until either discharge from ED or hospital.
Outcomes:
- Primary Outcomes: Time from medication administration to RASS ≤ -1 (adequate sedation)
-
Secondary Outcomes:
- Need for rescue medications
- Occurrence of prespecified adverse events:
- Apnea treated with bag-valve mask ventilation
- Laryngospasm
- Requirement of supplemental oxygen
- Dystonia
- Occurrence of Neuroleptic Malignant Syndrome within 72 hours
Inclusion Criteria:
- Adults 19-60 years of age
- Severe Psychomotor agitation measured by RASS ≥ +3
Exclusion Criteria:
- Previous enrollment in this study
- In police custody
- Known pregnancy or breastfeeding state
- Known hypersensitivity, intolerance, or allergy to study medications
- Specified comorbid conditions:
- Narrow angle glaucoma
- COPD
- Acute pulmonary insufficiency
- Severe cardiac decompensation
- Significant hypertension
- CVA
- Parkinson’s disease
- Severe depressive states and spastic diseases
Results:
- 80 patients enrolled and randomized equally to 2 study arms
- 68% of patients were men
- Median age = 35 years
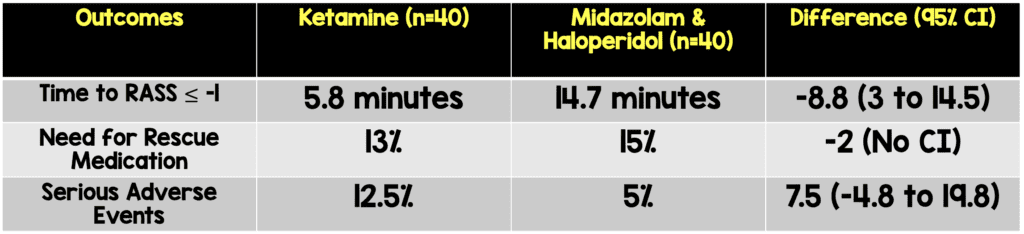
- Primary Outcome:
-
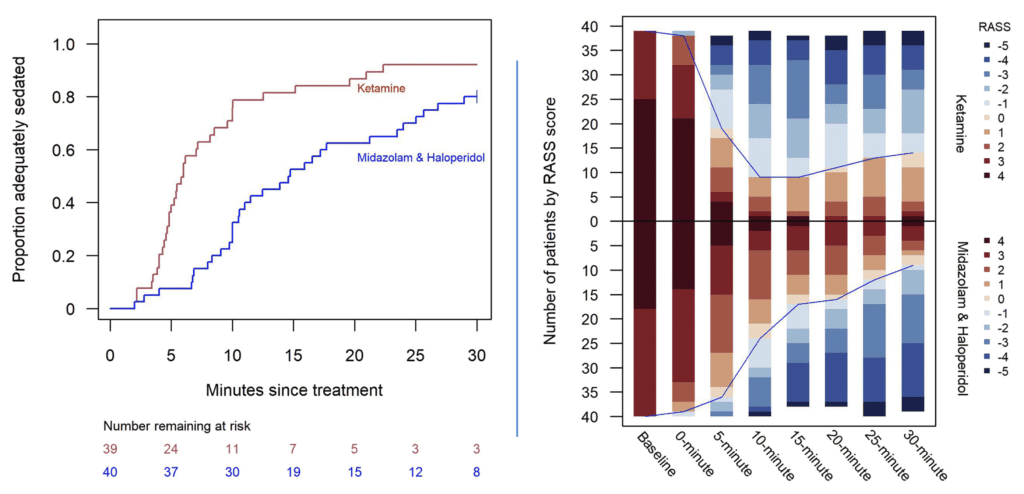
- Time to RASS ≤ -1 (adequate sedation): Time to adequate sedation was shorter in the ketamine arm and at each 5-minuate interval, a greater proportion of patients receiving ketamine achieved adequate sedation versus midazolam and haloperidol.
-
Secondary Outcomes:
- Need for rescue medications: The proportion of patients requiring rescue medications was similar in both arms.
- Occurrence of prespecified adverse events: More patients in the ketamine arm experienced adverse effects compared to midazolam and haloperidol.
- No patients required endotracheal intubation or ICU admission
Strengths:
- Adds further information to a question with inconsistent previous research during a time where ketamine is being scrutinized in regard to its use in the Emergency Department.
- Prospective, randomized clinical trial
- Group allocation was blinded to staff, study investigators, research assistants, and patients
- 2 independent ED physicians adjudicated all potentially serious adverse events
Limitations:
- Single center study
- Convenience sample (patients only enrolled from 8am till midnight) could cause a selection bias.
- The trial did not achieve prespecified enrollment target with overall small sample size causing wide confidence intervals in all outcomes.
- The trial was halted early due to a moratorium on in-person clinical research during the COVID-19 pandemic which did not allow for sufficient sample size to achieve adequate power.
- Comparison of Ketamine versus a combination of midazolam and haloperidol. Multiple other benzodiazepine and antipsychotic combinations are routinely used and at different doses which may yield different results.
- One nurse, who was not collecting data was unblinded to medications. This could result in unblinding.
- Ketamine was split into multiple syringes whereas midazolam and haloperidol were given as a single intramuscular injection. Another potential for unblinding.
- One issue not discussed in this trial is the length of time it took patients to be able to talk to the psychiatry team for a disposition. In other words, we want a medication that quickly and safely reduces agitation on the front end but doesn’t act so long that it delays disposition on the back end.
- Rescue medication necessity was at the discretion of the attending physician. If study became unblinded this could affect the results of this outcome.
- Groups unbalanced with more patients in the ketamine group with initial RASS ≥4 (64.1% vs 45.0%). This could diminish the effectiveness in the ketamine group as patients were more agitated at baseline.
Discussion:
- The authors note that they observed a statistically significant and clinically relevant shorter time to adequate sedation with the use of intramuscular ketamine.
- They additionally stated that there was no difference in the use of rescue medications between the two treatment arms and that despite a higher percentage of adverse effects in the ketamine group, overall, they were infrequent and managed without lasting sequelae.
- They note that 5 patients in the ketamine arm versus 2 patients in the midazolam and haloperidol overall experienced adverse events and that due to the sample size, this study did not have sufficient power to assess potential differences in safety.
- Interesting, this study utilized 5mg of midazolam IM as most people will use 2mg along with 5mg of haloperidol. Despite using a higher dose of midazolam there was no increase in adverse events (although the study was not powered adequately to look at this outcome).
- This is an important study that is attempting to clarify the evidence-based nature of ketamine use in the emergency department in patients with acute agitation. Currently, the 2017 ACEP guidelines give no level A or B recommendation on the use of ketamine and a level C consensus recommendation exists that classifies ketamine as a possible option for the severely agitated patient. Hopefully this study will further help and serve as a jumping off point for further research into identifying and clarifying the role of ketamine for severe psychomotor agitation in the emergency department.
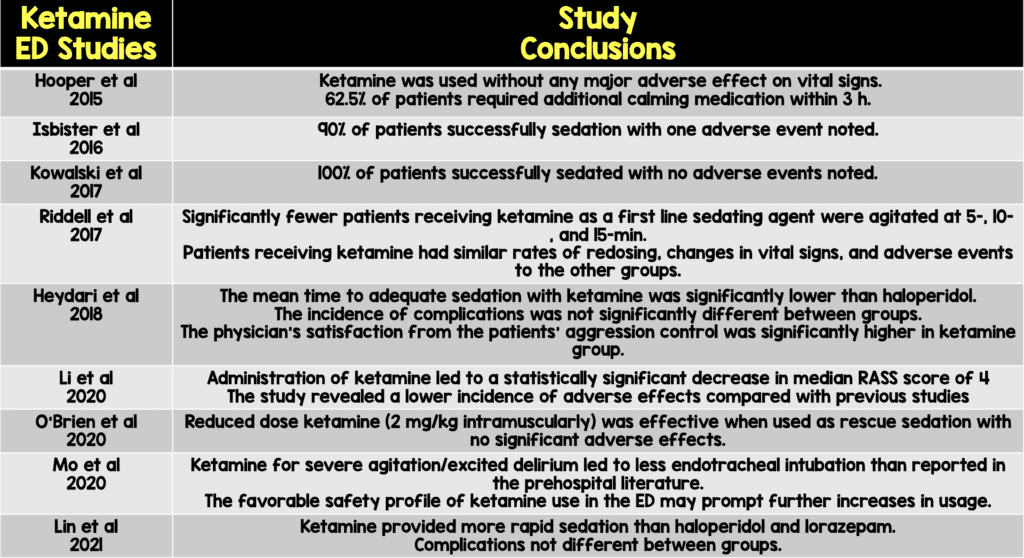
- Ketamine has previously been evaluated for control of severe agitation in the emergency department settings, providing a basis of evidence supporting its use. To date, the following studies on ketamine summarized below have been conducted in the emergency department. Overall, they trend towards ketamine being a safe and effective medication for the use of severe psychomotor agitation in the emergency department.
Author Conclusion:
“Ketamine achieves faster sedation of severely agitated ED patients while maintaining a similar safety profile.”
Clinical Take Home Point:
In this small randomized clinical trial of patients with severe psychomotor agitation, the use of ketamine was associated with a significantly shorter time to adequate sedation versus a combination of midazolam and haloperidol. The findings need to be interpreted in the context of an inadequate number of enrolled patients, early termination of the trial, and single center setting.
The bottom line is that the use of ketamine appears to be a safe and attractive alternative with a good safety profile for severe psychomotor agitation in the emergency department.
References:
- Hopper AB et al. Ketamine use for acute agitation in the emergency department. J Emerg Med. 2015. PMID: 25843924
- Isbister GK et al. Ketamine as Rescue Treatment for Difficult-to-Sedate Severe Acute Behavioral Disturbance in the Emergency Department. Ann Emerg Med. 2016. PMID: 26899459
- Kowalski JM et al. A Novel Agent for Management of Agitated Delirium: A Case Series of Ketamine Utilization in the Pediatric Emergency Department. Pediatr Emerg Care. 2017. 26466151
- Riddell J et al. Ketamine as a first-line treatment for severely agitated emergency department patients. Am J Emerg Med. 2017. PMID: 28237385
- Heydari F et al. Effect of Intramuscular Ketamine versus Haloperidol on Short-Term Control of Severe Agitated Patients in Emergency Department; A Randomized Clinical Trial. Bull Emerg Trauma. 2018. PMID: 30402516
- Li M et al. Evaluation of Ketamine for Excited Delirium Syndrome in the Adult Emergency Department. J Emerg Med. 2020. PMID: 31735659
- O’Brien ME et al. Reduced-dose intramuscular ketamine for severe agitation in an academic emergency department. Clin Toxicol (Phila). 2020. PMID: 31335216
- Mo H et al. Ketamine Safety and Use in the Emergency Department for Pain and Agitation/Delirium: A Health System Experience. West J Emerg Med. 2020. PMID: 31999250
- Lin J et al. Efficacy of ketamine for initial control of acute agitation in the emergency department: A randomized study. Am J Emerg Med. 2021. PMID: 32340820
Post Peer Reviewed By: Salim R. Rezaie, MD (Twitter: @srrezaie)
The post Rapid Agitation Control With Ketamine in the Emergency Department appeared first on REBEL EM - Emergency Medicine Blog.
