
 Background: In the ED, POCUS has become one of the most important tools in discovering both the diagnosis and in the management of critically ill patients. cardiac arrest, is ultimately as sick as a person can get in the spectrum of critical illness. I mean how can someone be deader than dead, right? There has been a slew of literature evaluating the use of POCUS in cardiac arrest and many providers have started to incorporate its use into their practice. Newer literature, however indicates that the use of POCUS prolongs CPR pauses which ultimately impacts good neurological survival. POCUS protocols may help decrease cognitive load, but many are too cumbersome and complicated. Enter the Cardiac Arrest Sonographic Assessment (CASA) exam.
Background: In the ED, POCUS has become one of the most important tools in discovering both the diagnosis and in the management of critically ill patients. cardiac arrest, is ultimately as sick as a person can get in the spectrum of critical illness. I mean how can someone be deader than dead, right? There has been a slew of literature evaluating the use of POCUS in cardiac arrest and many providers have started to incorporate its use into their practice. Newer literature, however indicates that the use of POCUS prolongs CPR pauses which ultimately impacts good neurological survival. POCUS protocols may help decrease cognitive load, but many are too cumbersome and complicated. Enter the Cardiac Arrest Sonographic Assessment (CASA) exam.
REBEL Cast Ep57 – Cardiac Arrest Sonographic Assessment (CASA) with Lead Author Kevin Gardner, MD
Click here for Direct Download of Podcast
What They Did: Description of a simplified POCUS algorithm during cardiac arrest. The exam consists of three, <10second POCUS exams during rhythm checks as shown in the image below. A phased array probe used in the subxiphoid view is the optimal view suggested as this view does not interrupt CPR. A key point is to have someone count out loud to not prolong CPR pauses and to record while ultrasounding so that images may be reviewed after resuming CPR. Finally, E-FAST can be performed on a case by case basis according to the authors.
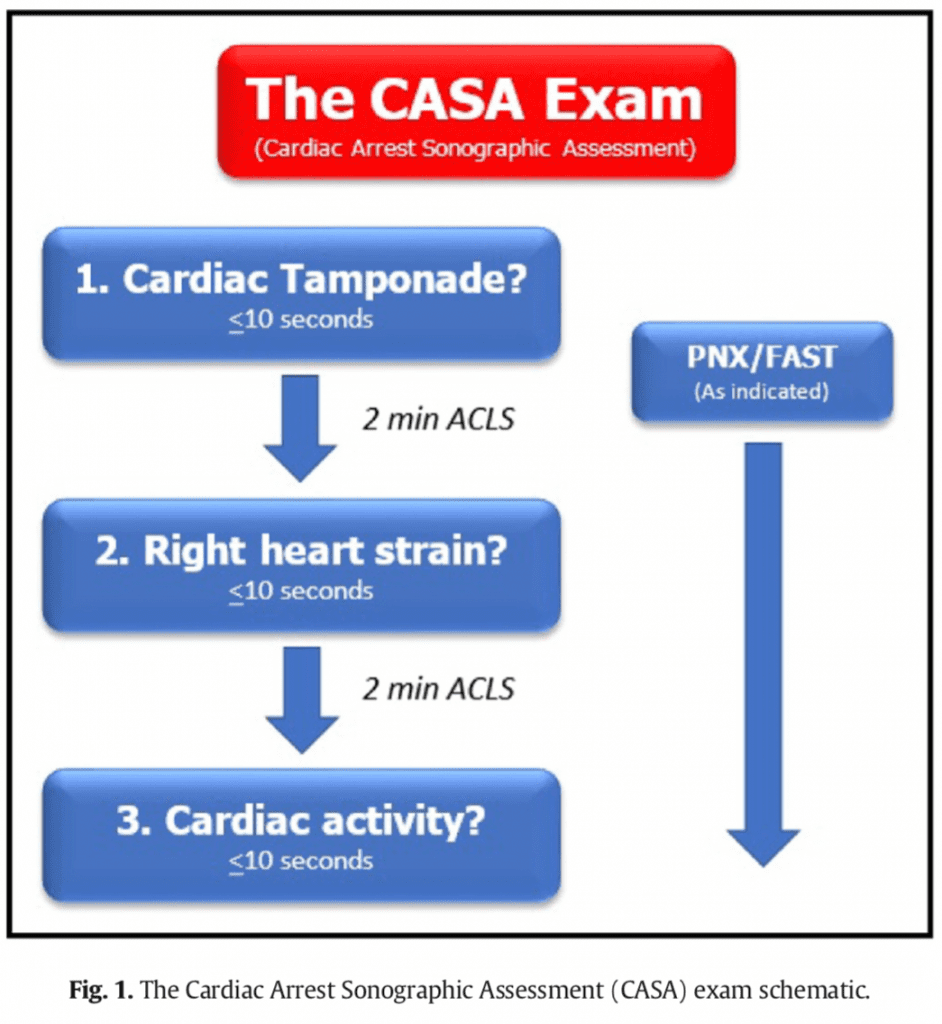
Step 1: According to the authors pericardial effusion causing cardiac tamponade is the cause of cardiac arrest in 4 – 15% of patients. Tamponade can be intervened upon with the use of pericardiocentesis.
Step 2: The authors state that, pulmonary embolism is the cause of cardiac arrest in 4.0 – 7.6% of patients. Evidence of right heart strain, should place pulmonary embolism higher in the differential, but there can be other causes of right heart strain. If PE is diagnosed, systemic thrombolysis is recommended.
Step 3: Finally, the authors state that the presence of absence of cardiac activity can provide useful prognostic information. Obviously the absence of cardiac activity in PEA portends worse outcomes (survival to hospital discharge rate = 0.0% – 0.6%). This finding along with other poor prognostic factors such as low end-tidal CO2, prolonged downtime, and unwitnessed arrest can help in the utility of ongoing resuscitation.
Ancillary Steps: Tension pneumothorax is a rare cause of non-traumatic cardiac arrest, but can be assessed by absence of lung sliding on POCUS in the anterior chest. If detected, needle decompression or finger/tube thoracostomy may be considered
Author Conclusion: “The CASA exam assesses for the highest yield reversible causes of PEA that can be visualized with ultrasound, while limiting POCUS’s negative impact.”
Interview with Lead Author Kevin Gardner, MD

Kevin F. Gardner, MD
Chief Resident
Department of Emergency Medicine
Highland Hospital – Alameda Health System
Oakland, CA, United States
The Idea for the CASA Exam
- Without a standardized POCUS protocol in cardiac arrest, US can cause harm by prolonging CPR pause duration
- Two Reasons this can Occur:
- Providers attempt to acquire too much information during rhythm checks
- Providers can be unsure which POCUS exam to perform without a priority list
- Both lead to confusion and inefficiency
- The CASA exam is a simple, streamlined POCUS protocol that can be performed the same way every time to increase efficiency and cognitively offload providers during a code
Type of US Probe and Location
- Ideally, use a phased array probe in the subxiphoid view
- While CPR is ongoing, place the probe in the subxiphoid view to get the heart into view (these images may not be perfect, but let you know where your probe needs to be during rhythm check)
- During the rhythm check, you are now already in position to acquire the images you need without causing further delays in compressions
- Every patients anatomy is different and the subxiphoid view may not be optimal, so other views may be required
- IMPORTANT POINT: Only one view should be attempted during each CPR pause (Attempting multiple views ultimately leads to prolonged CPR pauses)
Ensuring Compression Pauses are Not Prolonged (<10secs)
- Kevin uses an automated 10 second timer that counts out loud
- Anecdotally, for Kevin, provider countdowns tend to be slower than an automated timer, so if you don’t have one, make the countdown go to 6 – 8 seconds instead to ensure the pauses are not falsely prolonged
- Don’t record and analyze the US clips in real time. Instead record the 10 second clip and then do assessment and analyze the clip while CPR is ongoing
Why Tamponade, Right Heart Strain, and then Cardiac Activity
- CASA tries to mirror the reported prevalence of reversible causes of cardiac arrest
- Cardiac tamponade has the highest prevalence in the literature followed by PE, which is why these are the first two assessments in the CASA exam
- Cardiac activity is placed last, because the prognostic value at time zero in the ED is not 100, there is low inter-rater agreement on cardiac activity in the literature, and also wanted to prevent premature cessation of cardiac arrest
Differentiating Right Heart Strain from PE vs Cardiac Arrest Itself
- Having an enlarged RV is not 100% specific for PE
- RV is enlarged in cardiac arrest, but is enlarged most in patients with PE
- View RV dilatation in clinical context of patient:
- Young female on OCPs with RV dilatation = PE higher on differential
- Older gentleman with COPD with RV dilatation = PE lower on differential
- Not seeing any RV dilatation = Eliminates PE from differential
- Kevin uses a subjective RV:LV ratio in his practice, but agrees a 1:1 ratio would be adequate to consider PE in the correct clinical context
How Long into Cardiac Arrest Does Absence of Cardiac Activity Play a Role in Calling a Code
- Calling a code should not be made by lack of cardiac activity alone, but in conjunction with EtCO2, witnessed or unwitnessed arrest, as well as other factors that play into prognosis (i.e. PEA/Asystole vs VF/VT, prolonged downtime, etc…)
- Dependent on prognostic factors + lack of cardiac activity
- Prolonged downtime, unwitnessed arrest, EtCO2 < 20mmHg –> 3 rounds of CASA exam –> no cardiac activity –> reasonable to stop resuscitation
- Witnessed arrest, bystander CPR, EtCO2 > 20mmHg –> 3 rounds of CASA exam –> no cardiac activity –> resuscitate for longer amount of time
Follow Up Study to Original CASA Exam
- Follow up before and after study completed and presented at SAEM and submitted for publication (Not Yet Published)
- 1 year cardiac arrests with evaluation CPR pause duration without CASA exam
- 6 months of cardiac arrests with evaluation of CPR pause duration with CASA exam
- SPOILER ALERT: Use of CASA exam reduced CPR pause length by about 4 seconds. There was also an absolute increase in ROSC and survival to hospital admission rates, however these were not statistically significant
Final Thoughts from Kevin
- Big Take Home Message: US is a powerful tool, but should be used judiciously to not cause harm. The CASA exam achieves this, balance of identifying reversible causes while continuing high-quality CPR with minimal interruptions, which is the single most important thing we do for patients in cardiac arrest
Clinical Take Home Point: POCUS has become one of the most important tools in discovering both the diagnosis and in the management of critically ill patients. Newer literature, however indicates that the use of POCUS prolongs CPR pauses which ultimately impacts good neurological survival. POCUS protocols such as the CASA exam may help decrease cognitive load and minimize pauses.
References:
- Gardner, KF et al. The Cardiac Arrest Sonographic Assessment (CASA) Exam – A Standardized Approach to the use of Ultrasound in PEA. AJEM 2018. PMID: 28851499
Post Peer Reviewed By: Anand Swaminathan, MD (Twitter: @EMSwami)
The post REBEL Cast Ep57 – Cardiac Arrest Sonographic Assessment (CASA) with Lead Author Kevin Gardner, MD appeared first on REBEL EM - Emergency Medicine Blog.
