In this episode of REBEL Cast,I sit down with Richard Levitan and talk about some ideas from his experience in New York, where he spent 10 days during the surge of the COVID-19 pandemic. And the lessons he took away were, I think, invaluable for how we’re going to manage these patients going forward.
In this episode of REBEL Cast,I sit down with Richard Levitan and talk about some ideas from his experience in New York, where he spent 10 days during the surge of the COVID-19 pandemic. And the lessons he took away were, I think, invaluable for how we’re going to manage these patients going forward.
REBEL Cast Episode 80 – A New War Plan for COVID-19 with Richard Levitan, MD
Click here for Direct Download of Podcast
Richard Levitan, MD
Website: AirwayCam
Twitter: @airwaycam
- First class of Emergency Medicine residents at Bellevue Hospital (1990-1994), and subsequently worked in academic, high-volume, inner-city trauma hospitals in NYC and Philadelphia for 25 years (Bellevue, Lincoln, Penn, Einstein, Jefferson). Starting in 2012 he began working in rural, critical care access hospitals. He now balances this clinical activity with teaching courses, speaking engagements, and device development.
- In addition to the Airway Cam (1994), his inventions include the Levitan FPS optical stylet (Clarus Medical), the Control Cric (Pulmodyne Inc.), and the Universal Stylet Bougie (USB, Intersurgical Ltd.). He has been involved in numerous device development projects with various manufacturers. He did early design testing and wrote the first published paper on the I-gel supraglottic airway.
- Designed and built his own unique intubation manikins (with anatomic variation) for teaching laryngoscopy (the Airway Training Series), as well as a unique anatomically correct surgical model (The Airway Cam Surgical Trainer), which uses an inexpensive three-layer skin analogue.
- Published extensively on laryngoscopy and airway management, and holds an Adjunct Professor appointment at Dartmouth (Geisel) School of Medicine, as well as a Visiting Professor appointment at the University of Maryland School of Medicine.
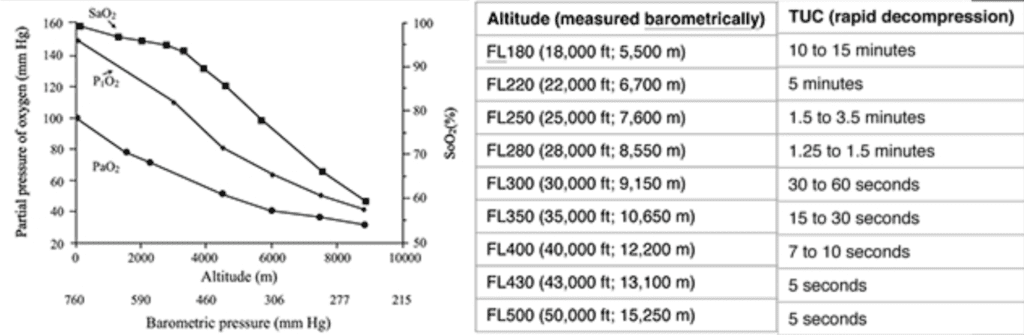
We are not calling this HAPE, but why is this important for us to understand people at altitude in the context of COVID-19 pathophysiology?
- COVID is caused by a respiratory virus, but what it does to the lungs is something that we have not seen before clinically. It causes a severe problem with oxygen absorption and we think that is because of collapse of alveoli due to its attack on the cells in the lungs that make surfactant (Alveolar type II cells).
- Despite the impaired oxygen absorption, patient’s lungs remain compliant. This is what Gattinoni refers to as the “type L” phase of COVID pneumonia.1
- There is only one endogenous physiologic response to hypoxia and that is to breathe faster. And we see this in people at high altitudes.
- The American Medical Research Expedition to Everest2 was an expedition where researchers drew blood gases on the summit of Everest. What was interesting was you had blood gases with PCO2 measurements of 15 mmHg or lower and PO2 measurements were in the 30’s. Clearly in severe respiratory alkalosis due to breathing so fast. When thinking about this in terms of the alveolar gas equation, the only way to improve oxygenation is to remove carbon dioxide by increase respiratory rate.
- We are seeing patients with respiratory rates of 40/min or higher and SpO2 measurements of 50-60%. What I believe is happening in COVID is patients are slowly getting hypoxic. They don’t feel it, because it’s not like a bacterial pneumonia that causes pain with breathing. It’s not subjectively appreciated by the patient, but they modify their respirations and increase their respiratory drive and minute ventilation in response to the hypoxia. This effectively blows off carbon dioxide, keeping them from subjectively feeling short of breath.
- Example from a patient I saw: pH- 7.68, PCO2- 16, PO2- 39, correlating with a SpO2 in the 50’s.
Clinical Phases of COVID Pneumonia:
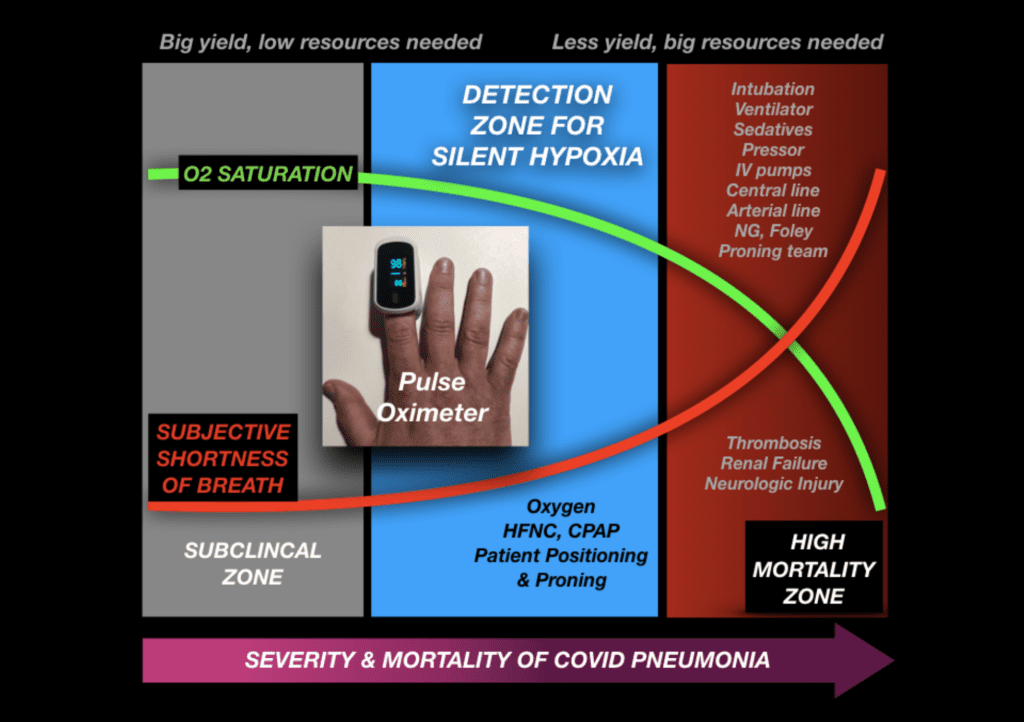
-
Subclinical zone
- O2 saturation is normal
- Respiratory rate is normal
-
Detection zone
- Gradual decline in O2 saturation
- No subjective shortness of breath, but respiratory rate begins to increase
- Progressive “self-inflicted lung injury” (SILI)
- This is where we can make a significant impact with treatment
-
High Mortality zone
- O2 saturation falls asymptotically
- Subjective shortness of breath rises asymptotically
- Transition from functional lungs with adequate PCO2 to the “type H” physiology where acute respiratory failure can occur suddenly.
-
My reasons for this framework:
- Patients come in with moderate to severe pneumonia with profound hypoxia. “I’ve been sick for days, but I became short of breath suddenly.” This is consistent with the “silent hypoxia” we are seeing that is corroborated with what I’m hearing from many patients and family members.
- The human brain can’t tolerate sudden significant drops in O2 We see this in aviation studies on “time of useful consciousness”.3
Thoughts on the “Happy Hypoxemic” Terminology:
- I prefer to use silent hypoxemia, these patients are not happy, they are dying from an incredibly slow onset of severe hypoxemia associated with hypocapnia.
How do we know when to intervene?
- We cannot rely on subjective shortness of breath due to physiological adaptations
- Ideally we should be monitoring patients with pulse oximetry and check in with them a few times a day
- Factors to consider:
- Oxygen saturation with a threshold of about ≈92 – 94%
- Note that this could be affected by elevation
- Patient variables that predict rapid deterioration (baseline atelectasis, eg: obesity, elderly, lung disease)
- Patients who deteriorate tend to do so in the 5 – 10d window. Therefore, knowing the time in the illness can predict further potential deterioration or improvement
- Inflammatory markers (D-dimer, ferritin, LDH, IL-6, etc…)
- Oxygen saturation with a threshold of about ≈92 – 94%
What treatment modalities should we use?
- HFNC + surgical mask
- Recruitment maneuvers
- Proning
- R/L lateral recumbency
- Sitting upright
- CPAP assistance
- Early steroids?
- Promising results and physiologically reasonable. But no concrete data yet.
What should our goals be?
- Intervene sooner to prevent alveolar collapse and inflammation
- Decrease work of breathing
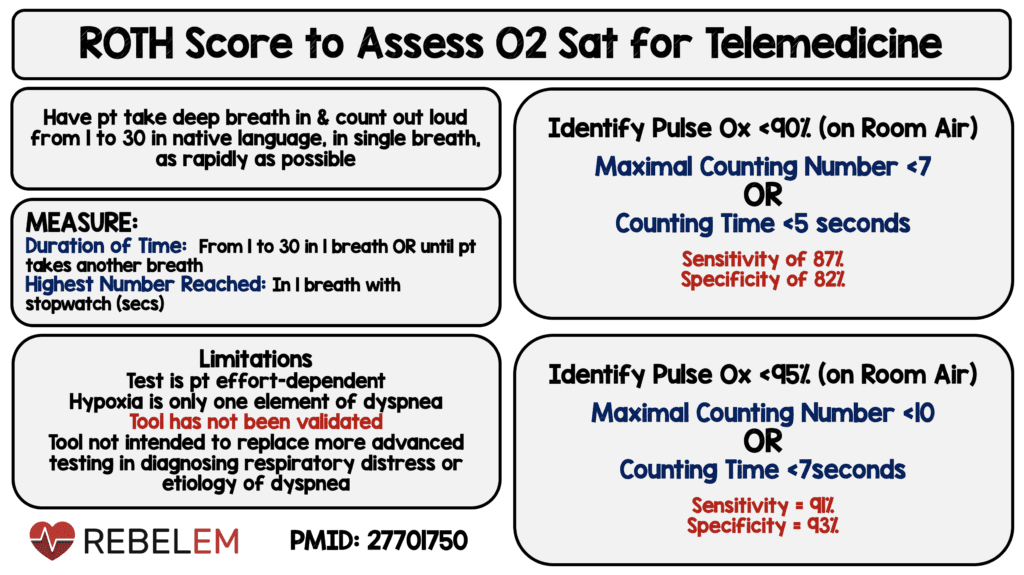
Should we consider using the Roth Score4?
- It doesn’t detect early silent hypoxia and isn’t as good at predicting subtle drops in O2 saturation
- We should find a way to get pulse oximeters out to the public. Examples:
- Distribute pulse oximeters for use at home
- Drive-by pulse oximetry for patients with mild symptoms of viral illness
- Pulse oximeters at pharmacies
Take Home Messages:
- Identify where patients are in their course of their illness and intervene earlier (i.e. day 1, 2….8, 9, 10, etc…)
- Before discharge:
- Lay patient flat on their back and check pulse oximetry to help with disposition decisions
- Give patient a pulse oximeter or have a method of checking in established
For More On This Topic Checkout:
- NY Times: The Infection That’s Silently Killing Coronavirus Patients
- CBS News: ER Doctor Shares What he Learned Volunteering at NY Hospital During Pandemic
References:
- Gattinoni L et al. COVID-19 pneumonia: different respiratory treatments for different phenotypes? Intensive Care Med 2020. PMCID: PMC7154064
- West J. American Medical Research Expedition to Everest. High Alt Med Biol 2010. PMID: 20586594
- Izraeli S et al. Determination of the “time of useful consciousness” (TUC) in repeated exposures to simulated altitude of 25,000 ft (7,620 m). Aviat Space Environ Med 1988. PMID: 3202796
- Chorin E et al. Assessment of Respiratory Distress by the Roth Score. Clin Cardiol 2016. PMID: 27701750
Transcript Written By: Yasien Eltigani, MS4 at St. George’s University (@yasieneltigani)
Post Peer Reviewed By: Anand Swaminathan, MD (Twitter: @EMSwami)
The post REBEL Cast Ep80: A New War Plan for COVID-19 with Richard Levitan appeared first on REBEL EM - Emergency Medicine Blog.