
 The standard treatment for patients with obstructive left main coronary artery disease has typically been coronary-artery bypass grafting (CABG), however some newer trials have suggested that maybe drug-eluting stents may be an acceptable alternative to CABG in select patients. In this episode we will be reviewing the two most recent publications on this topic:
The standard treatment for patients with obstructive left main coronary artery disease has typically been coronary-artery bypass grafting (CABG), however some newer trials have suggested that maybe drug-eluting stents may be an acceptable alternative to CABG in select patients. In this episode we will be reviewing the two most recent publications on this topic:
- The EXCEL Trial
- The NOBLE Trial
REBEL Cast Episode 31: Obstructive Left Main Coronary Artery Disease – PCI or CABG?
Click here for Direct Download of Podcast
The EXCEL Trial
What They Did:
- International, open-label, multicenter, randomized clinical trial of patients with left main coronary artery disease to undergo percutaneous coronary intervention (PCI) with a drug eluting stent or CABG
- Trial designed to determine whether PCI non9nferior to CABG
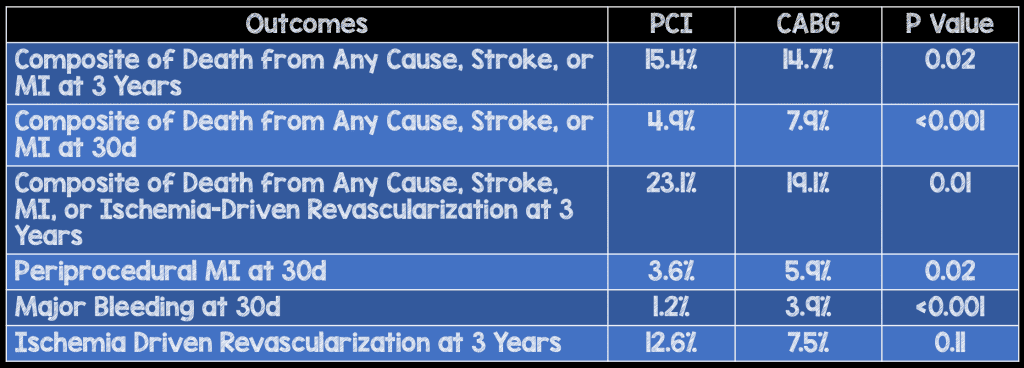
Outcomes:
- Primary Endpoint: Rate of composite outcome (Death from any cause, stroke, or myocardial infarction at 3 years)
- Secondary Endpoints:
- Rate of composite of death from any cause, stroke or myocardial infarction at 30 days
- Rate of a composite of death, stroke, myocardial infarction, or ischemia-driven revascularization at 3 years
Inclusion:
- Stenosis of the left main coronary artery of 70% or more
- Stenosis of 50% to less than 70% if determined by means of noninvasive or invasive testing to be hemodynamically significant
- Low to intermediate anatomical complexity of coronary artery disease, as defined by a site-determined SYTAX score of 32 or lower
Results:
- 2905 patients with left main coronary artery disease were recruited at 126 sites in 17 countries
- 1905 patients underwent randomization
- 948 PCI group
- 957 CABG group
Strengths:
- Multicenter, randomized control trial
- Randomization performed with use of an interactive voice-based or web-based system in block sizes of 16, 24, or 32
Limitations:
- Blinding of patients and investigators not possible
- Long-term medication use after PCI and CABG varied and it is not clear if these differences contributed to observed results
- This was only a 3-year follow up, but longer term follow up would be needed to see if there is a difference between PCI and CABG
- Initial 747 randomized patients were consecutive. Unclear if other randomized patients were enrolled consecutively.
Discussion:
- The 3-year rate of revascularization was 5% higher with PCI than with CABG (although symptomatic graft occlusion rate was higher than definite stent thrombosis [5.4% vs. 0.7%]), whereas the rate of early myocardial infarction and major adverse events (i.e. bleeding, infection, major arrhythmia, and renal failure) were 15% lower with PCI vs CABG
- SYNTAX score is something calculated at the time of heart catheterization and not something EM physicians can calculate at the time of evaluation in the ED.
Author Conclusion: “In patients with left main coronary artery disease and low or intermediate SYNTAX scores by site assessment, PCI with everolimus-eluting stents was noninferior to CABG with respect to the rate of the composite end point of death, stroke, or myocardial infarction at 3 years.”
Clinical Take Home Point: In select patients with left main coronary artery disease and a low to intermediate SYNTAX score, PCI with drug eluting stents was noninferior to CABG for the primary outcome of death, stroke or myocardial infarction at 3 years. This should be balanced with the increased revascularization rate at 3 years with PCI vs CABG.
The NOBLE Trial
What They Did:
- Prospective, Randomized, Open-Label, Non-Inferiority Trial
- 36 centers in northern Europe
- Patients with left main coronary artery disease randomized in a 1:1 treatment of PCI or CABG
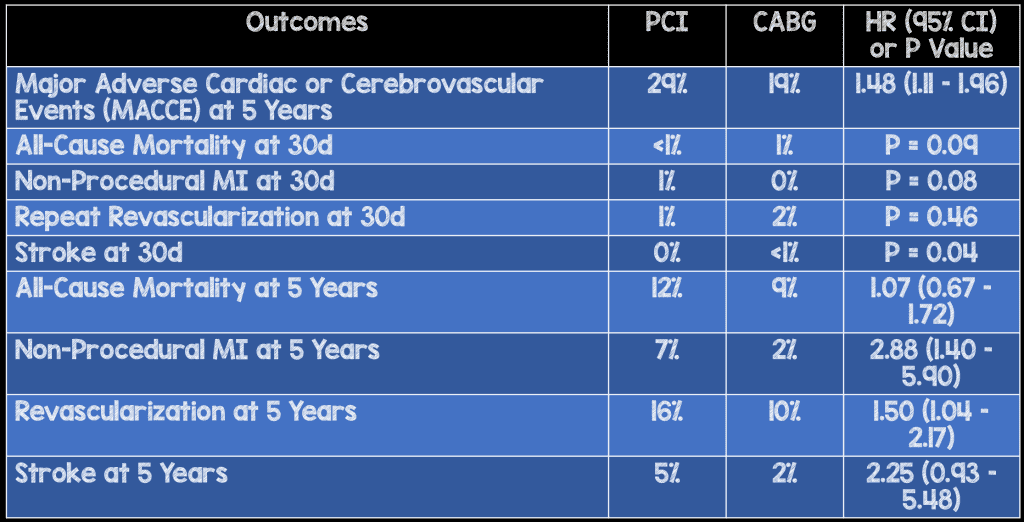
Outcomes:
- Primary Outcome: Major Adverse Cardiac or Cerebrovascular Events (MACCE) – Composite of All-Cause mortality, non-procedural myocardial infarction, any repeat coronary revascularization, and stroke
- Secondary Outcomes: Individual outcomes of all-cause mortality, non-procedural myocardial infarction, any repeat coronary revascularization, and stroke
Exclusion:
- ST-Elevation Myocardial Infarction (STEMI) within 24hrs
- Expected survival of <1 year
Results:
- 1201 Patients Enrolled (1192 Included in the analysis)
- 598 PCI
- 603 CABG
Strengths:
- Multicenter study
- Randomized Clinical Trial
- Clinically relevant patient oriented outcomes
Limitations :
- The number events needed to be reached at 2 years was not successful, therefore the follow-up period was extended to 5 years for MACCE
- Even though the median follow up period was 3.1 years, there was only a 38T and 35% follow up at 5 years for PCI and CABG cohorts respectively
- Patients in this trial were elective procedures, making generalization of results to patients in the acute, unstable setting difficult. These patients may be better suited for PCI over CABG.
- 11% of patients were treated with first-generation drug-eluting stents potentially diluting the PCI results, as first generation stents have more thickness and a higher rate of in-stent thrombosis compared to newer stents
- Combined primary endpoint where all endpoints are not equal (i.e. death not equal to revascularization)
Discussion:
- Key findings of the NOBLE Study:
- CABG better than PCI for composite endpoint of MACCE
- All-cause mortality similar between two groups
- Nonprocedural myocardial infarction and need for repeat vascularization were increased after PCI
- Higher rate of stroke observed in the CABG group after 30 days
- Major difference in favor of CABG in the revascularization outcome which may be subjective. Exclusion of revascularization from primary endpoint would significantly change the HR and move it towards non-inferiority as seen in EXCEL trial
Author Conclusion: “The findings of this study suggest that CABG might be better than PCI for treatment of left main stem coronary artery disease.”
Clinical Take Home Point: This study differs from the EXCEL trial in that CABG was shown to be better than PCI for treatment of left main stem coronary artery disease. This difference may be due to the different endpoints in the two studies (inclusion/exclusion of revascularization).
References:
- Stone GW et al. Everolimus-Eluting Stents or Bypass Surgery for Left Main Coronary Artery Disease. NEJM 2016. [Epub Ahead of Print]. PMID: 27797291
- Makikallio T et al. Percutaneous Coronary Angioplasty Versus Coronary Artery Bypass Grafting in Treatment of Unprotected Left Main Stenosis (NOBLE): A Prospective, Randomised, Open-Label, Non-Inferiority Trial. Lancet 2016. S0140 – 6736 (16): 32052 – 9. [Epub Ahead of Print]. PMID: 27810312
Post Peer Reviewed By: Anand Swaminathan (Twitter: @EMSwami) and Matt Astin (Twitter: @mastinmd)
The post REBEL Cast Episode 31: Obstructive Left Main Coronary Artery Disease appeared first on REBEL EM - Emergency Medicine Blog.
