
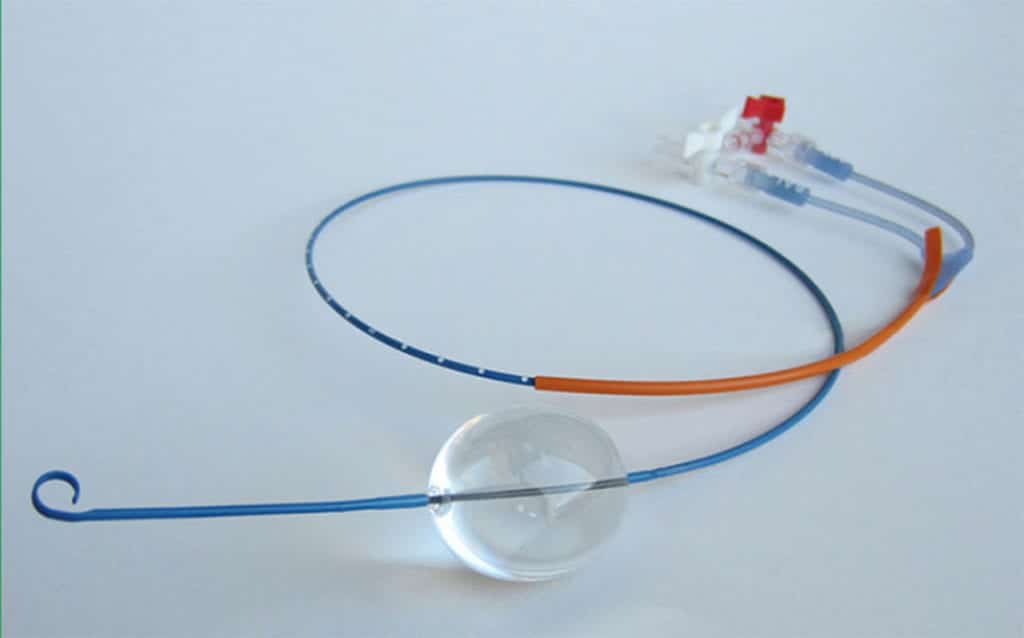
 The use of resuscitative endovascular balloon occlusion of the aorta (REBOA) has been a hot topic on the cutting edge of trauma resuscitation for several years now. But who should be doing this procedure, on whom, and when? Tissue ischemia results from REBOA followed by reperfusion injury, organ dysfunction and potential cardiovascular collapse. Although appropriate patient selection is paramount, the system of care that surrounds this procedure is vital to minimizing delays to definitive hemorrhage control as well as the ischemic insult of aortic occlusion.
The use of resuscitative endovascular balloon occlusion of the aorta (REBOA) has been a hot topic on the cutting edge of trauma resuscitation for several years now. But who should be doing this procedure, on whom, and when? Tissue ischemia results from REBOA followed by reperfusion injury, organ dysfunction and potential cardiovascular collapse. Although appropriate patient selection is paramount, the system of care that surrounds this procedure is vital to minimizing delays to definitive hemorrhage control as well as the ischemic insult of aortic occlusion.
In 2018, the American College of Surgeons Committee on Trauma (ACS COT) and the American College of Emergency Physicians (ACEP) published a joint statement on the clinical use of REBOA2. This statement was met with much criticism from the emergency medicine/critical care world. Due to this, a revised statement has been published with different recommendations1. So, what does this statement say and how is it different from the 2018 statement?
General Observations:
- No high-grade evidence demonstrating REBOA improves outcomes or survival (No Class I or II data) compared to standard treatment of severe traumatic hemorrhage
- The majority of hypotensive trauma patients will respond to resuscitation and will not need aortic occlusion
- Have to be careful comparing patients with hemorrhagic shock requiring emergent hemorrhage control procedures with and without REBOA as a selection bias for REBOA use in patients who fail to respond to resuscitation which confounds this comparison, usually favoring other hemorrhage control measures
- Most available evidence only report short term patient outcomes during the initial resuscitation period and neglect delayed complications and mortality
- Also, most data in the US comes from a small number of trauma centers with extensive experience with REBOA and these results may not be generalizable to all US EDs
- REBOA is a tool that should only be employed to temporize select patients at high risk of mortality from non-compressible torso hemorrhage as part of a larger system that includes damage control resuscitation, definitive hemorrhage control, and post-operative care (REBOA is not a definitive hemorrhage control device)
- Updated recommendations do not include the US military’s use of REBOA or address potential indications for REBOA outside of patients with traumatic hemorrhage
REBOA Utilization:
- May be used for traumatic life-threatening hemorrhage below the level of the diaphragm in those hemorrhagic shock patients refractory to resuscitation
- Does not confer any long-term survival advantage when used in traumatic cardiac arrest compared with standard care
- Contraindicated in major thoracic hemorrhage and pericardial tamponade
- Insufficient data on REBOA use in pediatric and geriatric populations
Complications:
- Prolonged ischemia can lead to fatal complications or spinal cord injury
- Reperfusion injury can lead to acute kidney injury and multisystem organ failure
- Mechanical complications can occur from femoral artery access and also injuries to the aorta and iliac artery (Arterial disruption, dissection, pseudoaneurysms, hematoma, thromboembolic events, and extremity ischemia)
- Overinflating the balloon can result in balloon rupture and/or iatrogenic aortic injury
- Prolonged attempts at getting vascular access, can delay definitive hemorrhage control
Guidelines for Use and Implementation:
- A multidisciplinary team approach is required providing continuity of care from the ED through to the ICU. All members of the team are required for protocols specific to environment of care and all team members need to be familiar with REBOA across the continuum of care
- “REBOA should only be placed by a surgeon or interventionalist responsible for definitive hemorrhage control or by a physician trained and qualified in REBOA in direct consultation with the physician who will provide definitive hemorrhage control.”
- The most common rate limiting step is safely and efficiently cannulating the common femoral artery (CFA) in hypovolemic patients. Use of ultrasound (the preferred method) or surgical cutdown are required
- Smaller diameter sheaths (<8 French) are associated with fewer limb complications
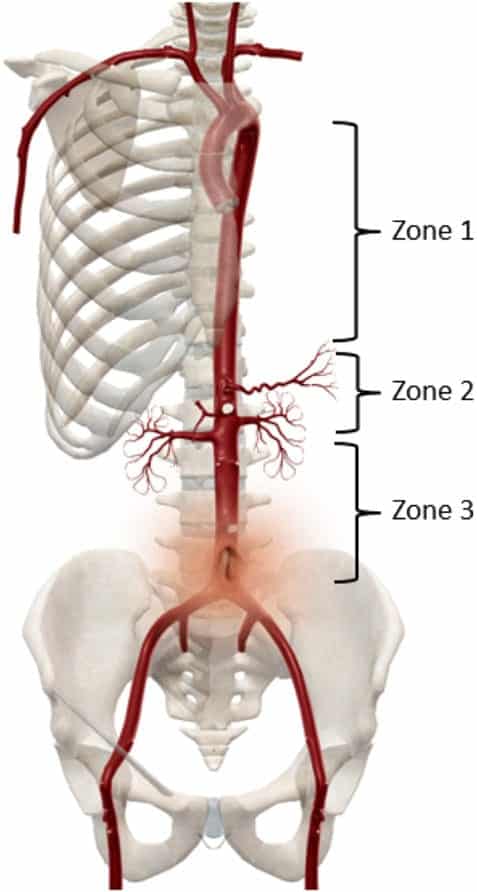
- Zone 1 (distal thoracic aorta) is used for severe intra-abdominal or retroperitoneal hemorrhage. Should not be used if cannot proceed to definitive hemorrhage control within 15 minutes. Total aortic occlusion times >30 min are associated with increased ischemic complications and risk of mortality
- Zone 3 (distal abdominal aorta) is used for isolated pelvic, junctional, or proximal lower extremity hemorrhage not amenable to tourniquet use. Should target ischemia time of less than 30 minutes, but no greater than 60 minutes
- Insufficient data to guide use of partial occlusion or intermittent inflation/deflation of the balloon.
- Vigilant assessment of lower extremity perfusion must occur before during, and after aortic occlusion and sheath removal for at least 24 hours after sheath removal
Systems of Care:
- If definitive hemorrhage control cannot be initiated in the recommended times above, systems should not use REBOA
- Interfacility transfer of REBOA patients is not recommended
- In EXTREMELY RARE circumstances in which patients with REBOA have immediate access to transportation and where the system can meet the time targets above for aortic occlusion to initiation of definitive hemorrhage control (<15min for Zone 1; <30min for Zone 3) interfacility transfer may be considered (This should include a direct to OR or IR policy, bypassing the ED)
- Prehospital use of REBOA in the US is not recommended (There is limited data on prehospital REBOA involving systems with physician-led teams that do not directly translate to the majority of current US EMS systems)
- In EXTREMELY RARE circumstances if there is a physician experienced in REBOA placement, is on scene, and the EMS system in partnership with the trauma system can meet the recommended time windows from aortic occlusion to the initiation of definitive hemorrhage control (<15min Zone 1; <30min Zone 3) pre-hospital REBOA may be considered
Differences from 2018 Statement:
- More input from emergency physicians (with and without critical care training)
- Additional input from prehospital clinicians, those involved with critical care transport, and military physicians
- Clarification on competency as opposed to specialty in placement of REBOA
- From the 2018 Consensus Statement: REBOA should only be performed by an acute care surgeon, vascular surgeon, or interventional radiologist trained in REBOA. EM physicians without critical care training should not perform REBOA
- From the 2019 Consensus Statement: “REBOA should only be placed by a surgeon or interventionalist responsible for definitive hemorrhage control or by a physician trained and qualified in REBOA in direct consultation with the physician who will provide definitive hemorrhage control.”
- Expansion and definition of training course requirements for successful use of REBOA (Very limited and highlighting only the BEST course in the 2018 statement)
Bottom Line:
REBOA is a useful tool in the treatment of life-threatening, non-compressible traumatic intra-abdominal hemorrhage in carefully selected patients. It is very resource intensive and is only a bridge therapy, much like ECMO. REBOA requires coordinated teamwork to get the patient from the emergency department to definitive hemorrhage control and post-operative care. This new statement opens this procedure up to emergency physicians to receive the training and become a part of these teams to help save the lives of our patients.
EXPERT Commentary:
It was a privilege to be involved in this process as a representative of ACEP. There had been a significant amount of disappointment and frustration with the initial statement, which had set off with good intention but in many people’s opinion a much too narrow inclusivity.
The second iteration was the result of a significant amount of work in reviewing the available limited quality data followed by a round-table evidence-based discussion. REBOA is a low-frequency but high-acuity procedure, and it is critical to be mindful of using it in the appropriate patient within the right system – just because you CAN do it doesn’t mean you should.
The revised statement highlights some key areas of use, and primarily aims to focus on competency as opposed to enforcing a siloed approach as the first statement did. I would emphasize that the key part of this is not so much who is doing it, but what is the system of care in which it is being done. Ultimately, the patient needs definitive hemorrhage control within a short period of time from occlusion – have you thought about the logistics of that? Implementation of this, as with similar high acuity low frequency procedures, requires a multidisciplinary approach to both training and implementation. This, I hope, is what the new statement emphasizes most.
We are continuing to learn and refine our approach to REBOA. What we thought was right 5 years ago may not be completely the same now. There are many naysayers, and some over-eager adopters. Is it for everyone? No. Are there a subset of patients who would otherwise die without it? Yes. The challenge is finding out if your system has a significant number of those latter patients to justify the development and use of this for you. Do a needs-assessment. Talk to your colleagues. See if this is right for your patients. If you proceed, then these guidelines can assist you in moving forward in a responsible manner. On our part, we will continue to revise the guidelines as newer evidence comes to light.
References:
- Bulger EM et al. Clinical use of Resuscitative Endovascular Balloon Occlusion of the Aorta (REBOA) in Civilian Trauma Systems in the USA, 2019: A Joint Statement from the American College of Surgeons Committee on Trauma, The American College of Emergency Physicians, The National Association of Emergency Medical Services Physicians and The National Association of Emergency Medical Technicians. Trauma Surg Acute Care Open 2019. PMID: 31673635
- Brenner M et al. Joint Statement from the American College of Surgeons Committee on Trauma (ACS COT) and The American College of Emergency Physicians (ACEP) Regarding the Clinical use of Resuscitative Endovascular Balloon Occlusion of the Aorta (REBOA). Trauma Surg Acute Care Open 2018. PMID: 29766135
Post Peer Reviewed By: Salim R. Rezaie, MD (Twitter: @srrezaie)
The post REBOA Time appeared first on REBEL EM - Emergency Medicine Blog.
