
 Definition: Medial or posterior slippage of the femoral capital epiphysis relative to the metaphysis
Definition: Medial or posterior slippage of the femoral capital epiphysis relative to the metaphysis
Epidemiology:
-
Classic patient group: overweight adolescent boys
- Over 80% of SCFE involves children with a BMI > 95th percentile (Manoff 2005).
- Average age of onset: 12 years old
-
Bilateral SCFE is fairly common
- 23% will have contralateral disease at the time of initial presentation, despite only complaining of unilateral pain (Hagglund 1988, Loder 1993).
- Up to 60% of patients will go on to develop bilateral SCFE in their lifetime
- 88% of subsequent slips occur within 18 months of diagnosing the first slip
- Influenced by bone maturation, strength, and weight mismatch.
- SCFE has also been associated with endocrine disorders such as hypothyroidism, hypogonadism, pan-hypopituitarism, but this is not as common.
Presentation:
- Groin, hip and thigh pain most common (85%) – constant or intermittent
- Isolated knee pain (15%)
- Limited internal rotation
- +/- Limp
- Immobility or refusal to bear weight
- Weakness
- Abnormal gait alignment
- May have no complaints of pain at time of presentation/examination
Differential Diagnoses:
- Muscle strain
- Pelvic fracture
- Acute Rheumatic Fever
- Developmental dysplasia of hip
- Juvenile idiopathic arthritis
- Legg-Calve-Perthes disease
- Septic arthritis
- Transient synovitis
- Osteosarcoma
Complications:
-
Usually secondary to delays in diagnosis due to:
- Vague, nonspecific symptoms as discussed above or delayed patient presentation
-
Failure to obtain appropriate imaging
- SCFE can present as isolated knee or distal thigh pain in up to 15% of cases (Matava 1999).
-
Subtle diagnostic findings in mild cases missed by inexperienced radiologists or orthopedists
- One retrospective study showed SCFE to be the second most commonly missed pediatric orthopedic diagnosis behind fracture (Skaggs 2002)
- Numerous retrospective studies demonstrate that the average time of symptom onset to diagnosis is eight weeks
-
Subsequent complications
- Avascular necrosis (AVN) of the femoral head
- Femoroacetabular impingement (FAI)
- Limb-length discrepancy
- Decreased range of motion
- Osteoarthritis
Diagnosis:
-
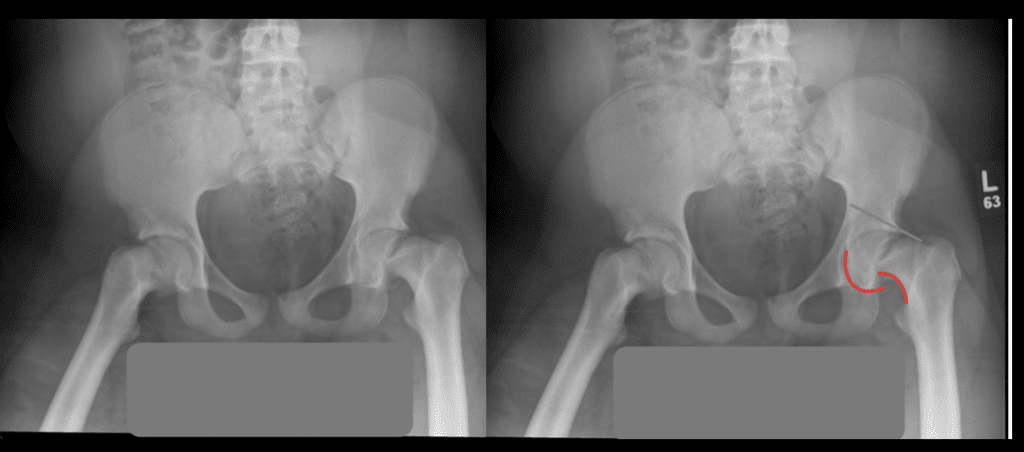
Plain Radiography (gold standard for diagnosis)
-
Views to obtain: XR Pelvis AP and Frog-Leg Lateral
- Bilateral imaging should be obtained due to the high rate of bilateral disease on initial presentation
-
SCFE identified on XR has been traditionally described as ice cream slipping off the cone
- Similar Salter Harris Type I Fracture due to disruption of physeal plate
-
Southwick Head Shaft Angle (SHSA) is used to classify the degree of slip
- Mild: < 30o
- Moderate: 31-50o
- Severe: > 51o
-
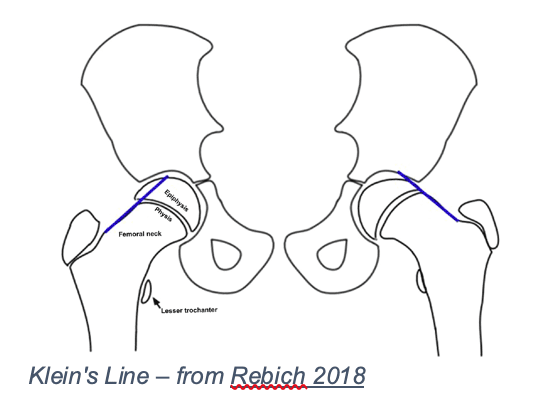
Klein’s Line/S-Sign
-
Klein’s Line
- Line drawn along the femoral neck and passes through the epiphysis.
- With SCFE, Klein’s Line does not include the epiphysis and instead will pass lateral to the epiphysis.
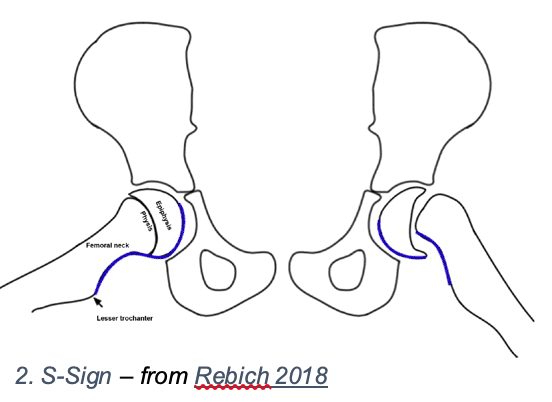
- S-Sign
- Smooth S-shaped line drawn along the femoral head-neck junction from lesser trochanter to the midpoint of the femoral head.
- If the line is asymmetric, discontinuous, or has sharp turns the likelihood of SCFE is significantly increased.
-
The combination of Klein’s line and the S-Sign are 96.5% sensitive and 85% specific for all cases of SCFE (Rebich 2018)
- Accurate and easily reproducible compared to SHSA making them more useful in early diagnosis and improving overall prognosis.
-
Klein’s Line
-
Views to obtain: XR Pelvis AP and Frog-Leg Lateral
-
Ultrasound
- 95% sensitivity (Magnano 1998)
- Can show hip effusion or metaphyseal step-off when radiographs are negative
- Operator dependent
- MRI
- Sensitivity as high as 88% (Magnano 1998).
- Useful in detecting early SCFE in “pre-slip” phase by identifying physeal abnormalities of those at risk of slippage even without radiographic evidence (Khaladkar 2015)
- CT
- Generally not indicated given the other available imaging modalities
- Avoid excessive and unnecessary radiation in children
Management:
- All patients should be immobilized and made non-weight bearing
- Obtain orthopedic consultation to determine need for early surgical intervention vs clinic referral for delayed repair
-
Simple (non-operative) closed reduction
- Contraindicated in stable SCFE
- Manipulation of an intact epiphyseal-metaphyseal interface without visualization can result in worsening instability and additional complications.
-
Identify avascular necrosis if present as this has been shown to be a complication of both delayed diagnosis as well as surgical repair of unstable SCFE
-
Preoperative
- MRI with contrast
- Bone scintigraphy
-
Intraoperative
- Visual confirmation of bleeding by drilling into femoral head
- Laser Doppler Flowmetry to measure pressure within the femoral head
-
Preoperative
-
Treatment options include open or closed surgical fixation via:
- Percutaneous in situ fixation
- Osteotomy
- Capsulotomy
Take Home Points
- Always consider SCFE in the differential diagnosis of a patient with non-traumatic hip, groin, thigh or knee pain
- Early recognition and diagnosis are crucial to avoid complications
- Immediate immobilization and urgent orthopedic consultation is crucial in management
- Surgical repair is the only definitive treatment modality
Guest Post By

C. Blair Gaines, MD
Emergency Medicine, PGY-3
Jackson Memorial Hospital
Miami, FL
References
- Asad I et al. Point-of-Care Ultrasound Diagnosis of Slipped Capital Femoral Epiphysis. Clin Pract Cases Emerg Med 2019. PMID: 30775677
- Kim TY et al. Limping: Evaluation, Diagnosis, and Management in the Pediatric ED. Pediatric Emergency Medicine Practice 2006. [Link is HERE]
- Lien J et al. Pediatric Orthopedic Injuries: Evidence-Based Management in the Emergency Department. Pediatric Emergency Medicine Practice 2017. PMID: 28825959
- Millis MB. SCFE: Clinical Aspects, Diagnosis, and Classification. Journal of Children’s Orthopaedics 2017. PMID: 28529655
- Otani T et al. Diagnosis and Treatment of Slipped Capital Femoral Epiphysis: Recent Trends to Note. Journal of Orthopedic Science 2018. PMID: 29361376
- Rahme D et al. Consequences of Diagnostic Delays in Slipped Capital Femoral Epiphysis. Journal of Pediatric Orthopaedics 2006. PMID: 16436942
- Rebich EJ et al. The S Sign: A New Radiographic Tool to Aid in the Diagnosis of Slipped Capital Femoral Epiphysis. JEM 2018. PMID: 29550284
Post Peer Reviewed By: Anand Swaminathan, MD (Twitter: @EMSwami) and Salim R. Rezaie, MD (Twitter: @srrezaie)
The post Slipped Capital Femoral Epiphysis (SCFE) appeared first on REBEL EM - Emergency Medicine Blog.
