
 Essentials of Emergency Medicine 2019 is taking place at the Cosmopolitan Hotel/Casino in Las Vegas, NV. I was asked to give five lectures on varying topics and wanted to share what was discussed at each of these sessions. If you haven’t been to Essentials of Emergency Medicine, you need to add this conference to your list of conferences to attend. The organizers pride themselves in discussing the latest practice-changing research and have meticulously designed content to maximize enjoyment and retention. In my humble opinion this conference is the quintessential medutainment extravaganza that applies learning theory principles, with amazing speakers, to provide you with the latest and greatest for clinical practice.
Essentials of Emergency Medicine 2019 is taking place at the Cosmopolitan Hotel/Casino in Las Vegas, NV. I was asked to give five lectures on varying topics and wanted to share what was discussed at each of these sessions. If you haven’t been to Essentials of Emergency Medicine, you need to add this conference to your list of conferences to attend. The organizers pride themselves in discussing the latest practice-changing research and have meticulously designed content to maximize enjoyment and retention. In my humble opinion this conference is the quintessential medutainment extravaganza that applies learning theory principles, with amazing speakers, to provide you with the latest and greatest for clinical practice.
The Literature Behind the Rule: PECARN Pediatric Head CT Algorithm
 In 2009 Kuppermann et al published their derivation and validation of the PECARN Pediatric Head CT Rule to minimize CT scan utilization while not missing clinically important traumatic brain injury. The rule was divided into patients <2 years of age and patients ≥ 2years of age.
In 2009 Kuppermann et al published their derivation and validation of the PECARN Pediatric Head CT Rule to minimize CT scan utilization while not missing clinically important traumatic brain injury. The rule was divided into patients <2 years of age and patients ≥ 2years of age.
Between 2007 – 2015 head CT use hasn’t changed much despite validated clinical decision rules being published [1]. The vast majority of these patients will suffer only a minor head injury which is nonfatal and does not warrant neurosurgery. However, it is estimated the rate of lethal malignancies from head CT is between 1 in 1000 and 1 in 5000 pediatric head CT scans with increasing risk at younger ages.
PECARN Pediatric Head CT Rules
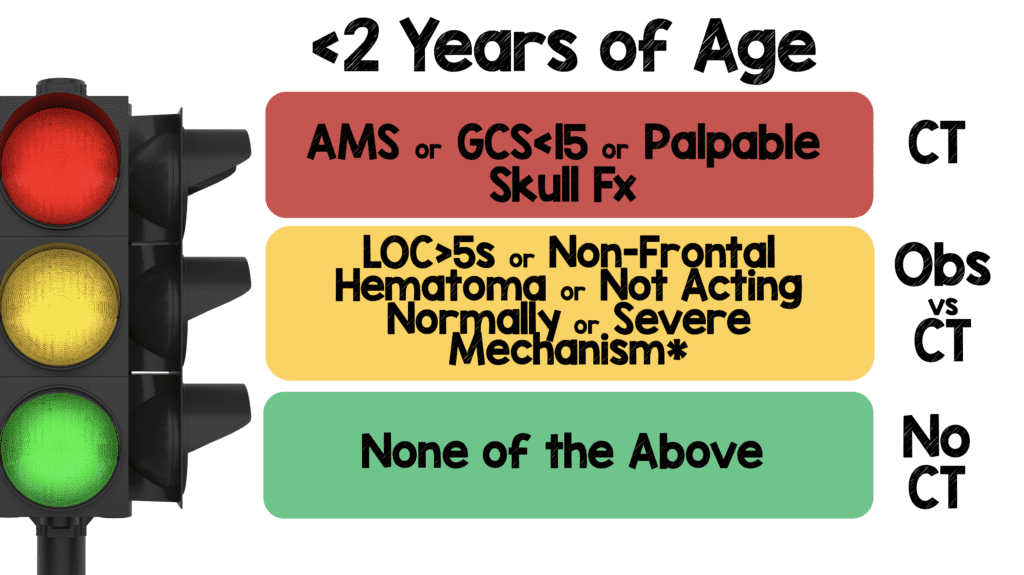
If a patient younger than 2 years of age has AMS or GCS < 15 or a Palpable Skull Fracture, then Head CT is recommended. If none are present, then the next tier is to see if the patient has LOC > 5 seconds, or a non-frontal hematoma, or is not acting normally or underwent a severe mechanism. If any criteria in this tier were met, then admission for observation should be considered, or a head CT could be considered based on clinician’s judgement. Shared decision making with the family is recommended. Finally, if none of the above criteria are present, then patient can be safely discharged home without imaging.
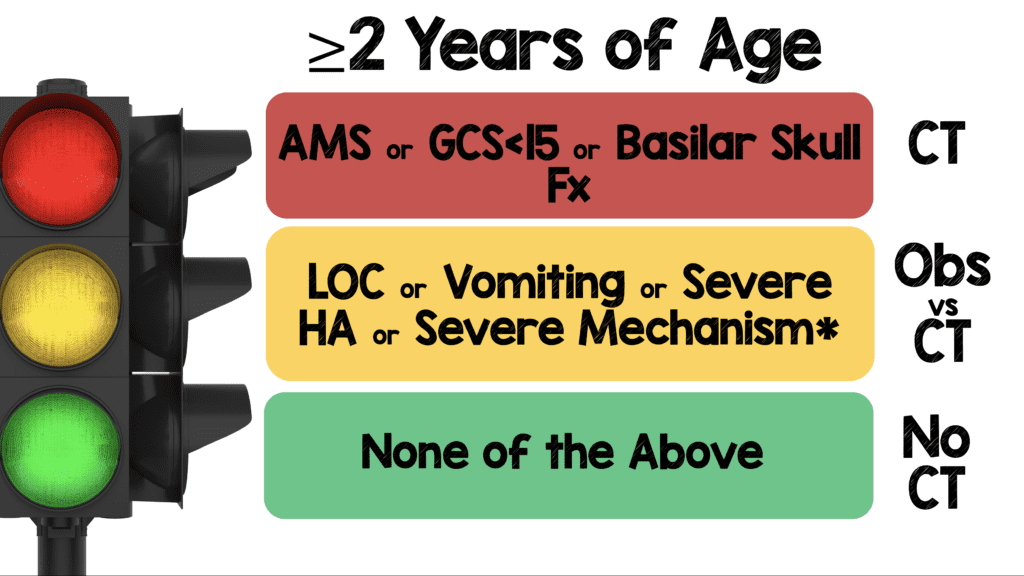
If patient ≥2 years of age has AMS or GCS < 15 or Signs of Basilar Skull Fracture, then Head CT is recommended. If none are present, then the next tier is to see if patient had LOC or vomiting or “severe headache” or a severe mechanism. In this middle tier, again admission for observation or head CT should be considered based on clinician judgement with shared decision making. Finally, if none of the above are present, then the patient can be safely discharged home without imaging. Before moving onto the results, there a few definitions that are important to understand before applying these rules:
Severe Mechanism per Kuppermann et al [2]:
- MVC + Ejection from the Vehicle
- MVC + Rollover
- MVC vs Pedestrian
- MVC + Death at the Scene
- High Impact Object
- Fall > 3ft (< 2years of age) or Fall >5ft (≥2 years of age)
Clinically Important Traumatic Brain Injury (ciTBI) per Kuppermann et al [2]:
- Death due to TBI
- Neurosurgery due to TBI
- Intubation >24hrs due to TBI
- Admission to Hospital >2 Nights due to TBI
What Were the Results of the Kuppermann et al [2]:
- > 42,000 patients were available for analysis (25% were <2 years of age)
- In the <2-year-old cohort:
- 1 ciTBI was missed, but none missed in validation group (Did not die or require neurosurgery)
- CT was obtained in 31.0% of derivation cohort and 31.3% in validation cohort
- Of these CTs 25.4% in the derivation cohort and 24.1% in the validation cohort had none of the 6 predictors of ciTBI
- In validation group:
- Sensitivity = 100% (86.3 – 100.0)
- NPV = 100% (95% CI 99.7 – 100.0)
- In the ≥2-year-old cohort:
- 9 ciTBIs were missed, but only 2 missed in validation group (none died or required neurosurgery)
- CT obtained in 37.3% of derivation cohort and 34.7% in the validation cohort
- Of these CTs 21.1% in the derivation cohort and 20.1% in the validation cohort had none of the 6 predictors of ciTBI
- In Validation group:
- Sensitivity: 96.8% (95% CI 89.0 – 99.6)
- NPV: 99.95% (95% CI 99.81 – 99.99)
Are There Other Validation Trials?
There are 6 more trials that I could find that divided children with head trauma into <2 years of age and ≥2 years of age. I excluded the Nakhjavan-Shahraki 2017 study because it was done in a resource limited country and had very small numbers.
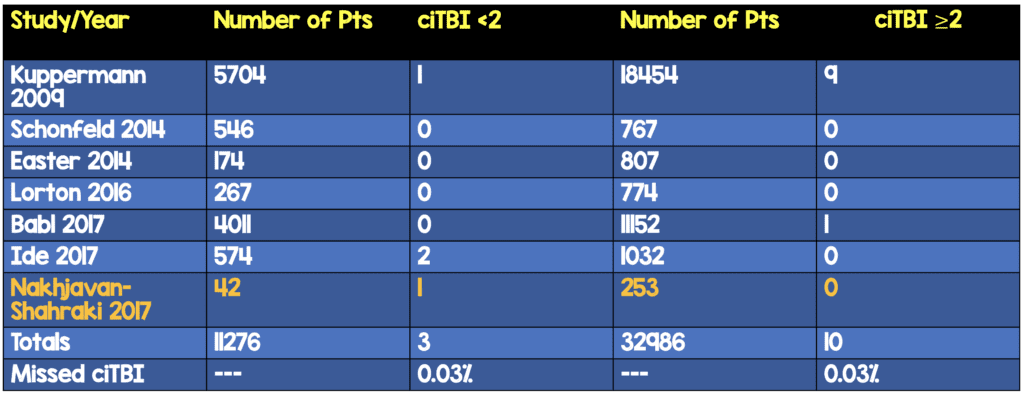
None of these trials missed any patients with death or need for neurosurgery due to TBI. All the missed cases required admission and observation.
The < 3 Month Old CAVEAT:
Patients < 3months old are not a well studied population. In the Kuppermann et al paper [2], the authors state:
“CT should be more strongly considered for children with multiple findings, worsening symptoms or signs, and for infants younger than 3 months.”
The reasons for this include, a thinner skull and less interaction, making it difficult to assess this age group.
Clinical Bottom Line: Using the PECARN Pediatric Head CT Rule has the potential to reduce unnecessary CT utilization while minimizing missed clinically important traumatic brain injuries (CAVEAT: Consider having a higher threshold for scanning children < 3months of age).
References:
- Burstein B et al. Use of CT for Head Trauma: 2007 – 2015. Pediatrics 2018. PMID: 30181120
- Kuppermann N et al. Identification of Children at Very Low Risk of Clinically-Important Brain Injuries After Head Trauma: A Prospective Cohort Study. Lancet 2009. PMID: 19758692
- Schonfeld D et al. Pediatric Emergency Care Applied Research Network Head Injury Clinical Prediction Rules are Reliable in Practice. Arch Dis Child 2014. PMID: 24431418
- Easter JS et al. Comparison of PECARN, CATCH, and CHALICE Rules for Children with Minor Head Injury: A Prospective Cohort Study. Ann Emerg Med 2014. PMID: 24635987
- Lorton F et al. Validation of the PECARN Clinical Decision Rule for Children with Minor Head Trauma: A French Multicenter Prospective Study. Scand J Trauma Resusc Emerg Med 2016. PMID: 27488722
- Babl FE et al. Accuracy of PECARN, CATCH, and CHALICE Head Injury Decision Rules in Children: A Prospective Cohort Study. Lancet 2017. PMID: 28410792
- Ide K et al. External Validation of the PECARN Head Trauma Prediction Rules in Japan. Acad Emerg Med 2017. PMID: 27862642
- Nakhjavan-Shahraki B et al. Pediatric emergency Care Applied Research Network (PECARN) Prediction Rules in Identifying High Risk Children with Mild Traumatic Brain Injury. Eur J Trauma Emerg Surg 2017. PMID: 28643031
Post Peer Reviewed By: Anand Swaminathan, MD (Twitter: @EMSwami)
The post The REBEL at Essentials of Emergency Medicine 2019 – Day 3 appeared first on REBEL EM - Emergency Medicine Blog.
