
 Background: Occlusion myocardial infarction (OMI) is defined as acute coronary occlusion or near occlusion with insufficient collateral circulation leading to downstream myocardial infarction. Currently, we use STEMI ECG criteria to identify acute coronary OMI in the clinical setting. The diagnosis of STEMI is based on millimeter criteria on the ECG (see below) and essentially acts as a surrogate marker for the presence of an OMI. Under the current STEMI vs NSTEMI paradigm, almost 1/3rd of NSTEMI patients have unrecognized acute total occlusion (OMI) discovered on delayed angiograms. The delay in diagnosis results in increased short and long-term mortality compared to NSTEMI patients without OMI (We have reviewed these trials before on REBEL EM). As ECG interpretation has improved it has become clear that there are other early ECG indicators of OMI that do not meet STEMI criteria (i.e. hyperacute T-waves) that would benefit from early percutaneous coronary intervention [2]. Additionally, there are other features such as hemodynamic instability and persistent symptoms, as well as adjunct modalities, like echocardiography, that can add useful information and increase the likelihood of OMI. Ultimately, the OMI paradigm emphasizes underlying pathology over surrogate test results (i.e. STEMI).
Background: Occlusion myocardial infarction (OMI) is defined as acute coronary occlusion or near occlusion with insufficient collateral circulation leading to downstream myocardial infarction. Currently, we use STEMI ECG criteria to identify acute coronary OMI in the clinical setting. The diagnosis of STEMI is based on millimeter criteria on the ECG (see below) and essentially acts as a surrogate marker for the presence of an OMI. Under the current STEMI vs NSTEMI paradigm, almost 1/3rd of NSTEMI patients have unrecognized acute total occlusion (OMI) discovered on delayed angiograms. The delay in diagnosis results in increased short and long-term mortality compared to NSTEMI patients without OMI (We have reviewed these trials before on REBEL EM). As ECG interpretation has improved it has become clear that there are other early ECG indicators of OMI that do not meet STEMI criteria (i.e. hyperacute T-waves) that would benefit from early percutaneous coronary intervention [2]. Additionally, there are other features such as hemodynamic instability and persistent symptoms, as well as adjunct modalities, like echocardiography, that can add useful information and increase the likelihood of OMI. Ultimately, the OMI paradigm emphasizes underlying pathology over surrogate test results (i.e. STEMI).
The ACS Spectrum Using the OMI vs NOMI Paradigm
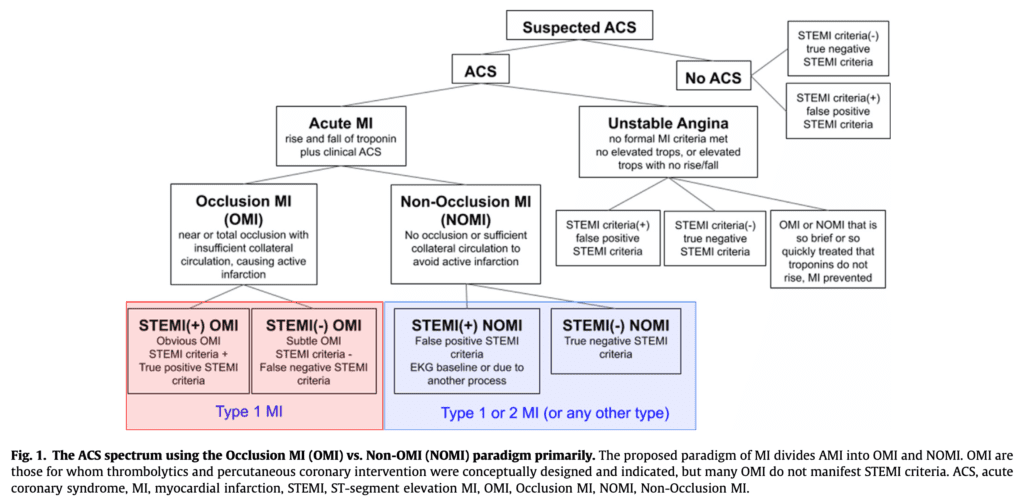
- STEMI = AMI with ECG findings meeting the definition of STEMI criteria in the fourth universal definition of MI
- STEMI (+) OMI = True Positive STEMI = Refers to patients with ECG features meeting formal STEMI criteria, who is found to have OMI as the cause of the STE and the AMI
- STEMI (-) OMI = Refers to OMI without the ECG meeting STEMI criteria (NSTEMI with occlusion)
- OMI = Refers to type 1 ACS involving acute occlusion or near occlusion of a major epicardial coronary vessel with insufficient collateral circulation, resulting in imminent necrosis of downstream myocardium without emergent reperfusion
- OMI is the anatomic and pathophysiologic substrate of STEMI, but not all OMI manifest as STEMI
Paper: Meyers HP et al. Accuracy of OMI ECG Findings Versus STEMI Criteria for Diagnosis of Acute Coronary Occlusion Myocardial Infarction. IJC Heart & Vasculature 2021. [Link is HERE]
Clinical Question: Are OMI ECG findings more accurate than STEMI Criteria for the diagnosis of Acute Coronary Occlusion MI (ACO MI)?
What They Did:
- Retrospective case-control study of patients with suspected acute coronary syndrome
- OMI Definition:
- Acute TIMI 0 – 2 flow culprit
- TIMI 3 flow culprit with peak troponin T ≥1.0 ng/mL or I ≥10.0ng/mL
- Compared the accuracy of ECG interpretation using predefined OMI ECG findings vs STEMI criteria for identification of OMI
Case Inclusion:
- Searched cardiac catheterization lab activation data base from both Stony Brook and Hennepin County:
- Presentation to the ED with symptoms suggestive of possible ACS
- Cardiac catheterization laboratory activation over past 1 year period
- Provided both cases (OMI) and controls (without OMI)
- From Stony Brook Only:
- Previously collected prospective population of ED patients admitted to cardiology service with suspected ACS (both controls and cases)
- From Hennepin County Only:
- Additional control patients with abnormal ECGs from Hennepin County without OMI but with STE, STD, or T-wave inversions
Case Exclusion:
- No ECGs in in EMR
- Insufficient retrospective information available to determine primary outcome (Presence or absence of OMI)
Results:
- 808 patients included
- 49% had AMI
- 33% OMI (41% of this portion met STEMI Criteria)
- 16% NOMI
- Angiography performed during index visit in 79% of cases
- 49% had AMI
- STEMI Criteria vs OMI Criteria
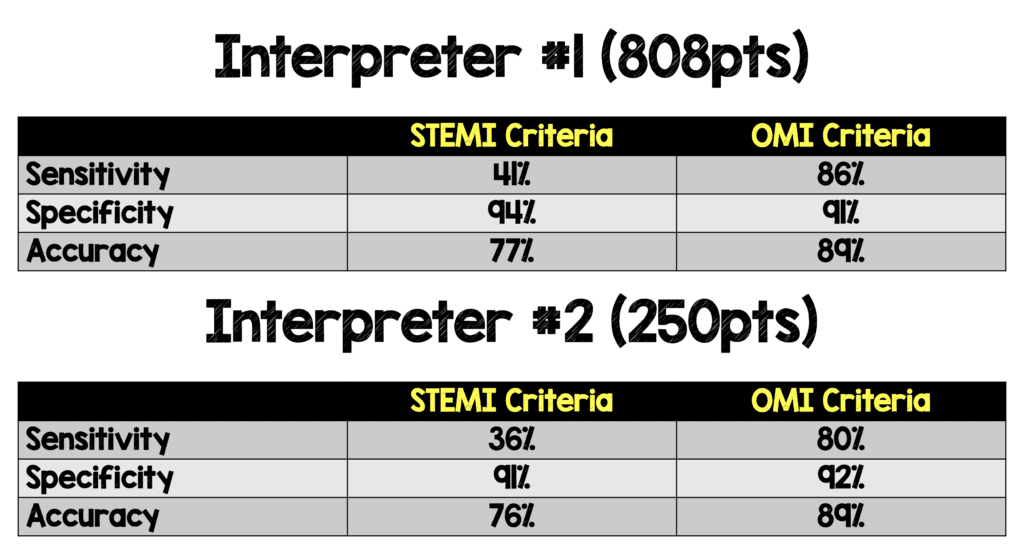
- Inter-rater reliability was excellent between interpreters 97.2% (k = 0.893) for determination of STEMI criteria and 94.0% (k = 0.849) for diagnosis of OMI
- Of the 265 OMI pts, 146 (55%) were diagnosed earlier using OMI ECG findings vs STEMI criteria)
- Average 3hrs earlier and median of 1.3hrs earlier by OMI ECG findings vs STEMI criteria or later angiogram
- Two most common OMI ECG findings (ECG could have multiple findings):
- Subtle STE not meeting STEMI criteria: 83%
- Reciprocal ST depression and/or reciprocal t-wave inversion: 82%
- 120 out of 146 never met STEMI criteria on any serial ECG recorded before angiogram
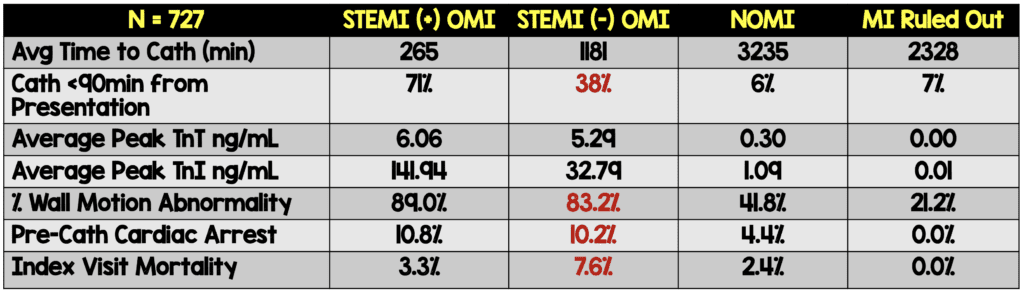
- STEMI (-) OMI patients had similar infarct size and mortality as STEMI (+) OMI patients, BUT had greater delays to angiography
- 727 patients had sufficient troponin data available
Strengths:
- Largest existing database containing angiographic outcome data, detailed ECG interpretation, peak cardiac troponin levels, echocardiography, and short-term mortality outcomes
- High inter-rater reliability of ECG interpretation
Limitations:
- ECG criteria are subjective and require experience for accurate interpretation and ultimately diagnosis.This can limit external validity based on the level of ECG interpretation. ECGs in this trial were interpreted by 2 experts with massive dedication of time/effort into ECG interpretation which will affect external validity to more novice ECG readers
- Convenience sample of patients which could create a selection bias.This can be seen by the high rate of STEMI and OMI in this cohort of patients (i.e. retrospective identification will miss cases)
- Selection bias in the fact that cases were collected from cath lab records.If you didn’t get a cath, you weren’t entered into the study
- ECG adjudication by study interpreters could have been biased in borderline cases in favor of STEMI (-) OMI.However, the authors asked a blinded cardiologist to also evaluate the ECGs to limit this bias. Through this blinding it was evident that study interpreters were more likely to call a STEMI compared to the cardiologist
- Long-term follow up data was not available, and a surrogate marker of infarct size was used (i.e. peak troponin level).Therefore, the long-term mortality, incidence of adverse events and quality of life in survivors was not reported
- There is also confounding in the fact that STEMI(+) patients get to the cath lab much quicker than STEMI (-) patients. Only a randomized clinical trial of immediate vs delayed angiography would be able to definitively answer this question.This will most likely not happen as it would not be ethically possible
Discussion:
- 146 (55%) of OMIs were POTENTIALLY correctly diagnosed a median of 1.5hrs earlier by OMI ECG findings than by either STEMI ECG criteria or by angiogram if ECG never met STEMI criteria (As this was not prospective, one cannot say that OMI criteria would definitively lead to earlier identification)
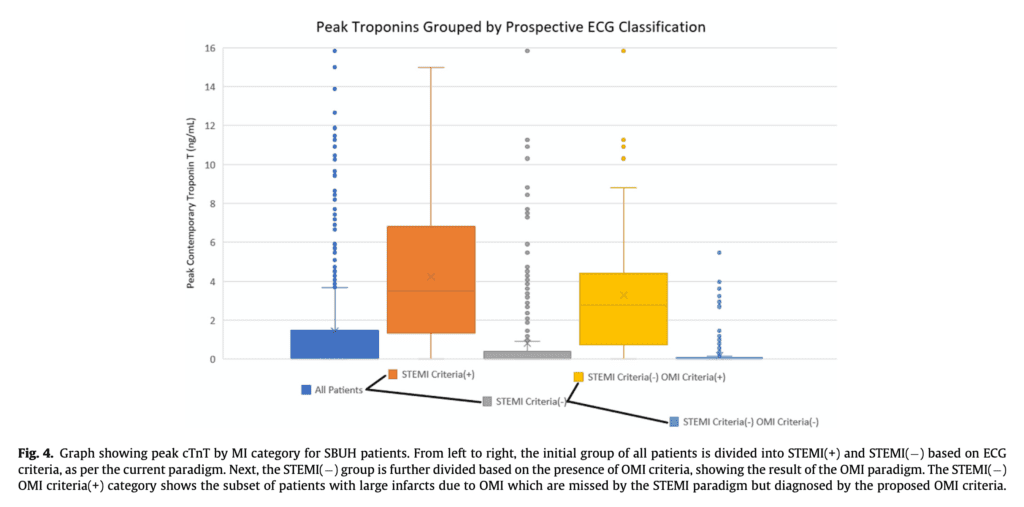
- Looking at the Stony Brook patient cohort, the authors break down coronary category and peak troponin level.The STEMI (-) OMI patients are very similar to STEMI (+) OMI patients (see below) in terms of peak troponin levels compared to the other groups.
- The specificity of OMI criteria was not significantly better than STEMI criteria for identifying “true positives.” However, there was a high rate of acute coronary lesions, elevated troponins and need for interventions in the OMI group compared to the STEMI criteria group.
- 51 cases with positive OMI ECG findings did not meet the primary outcome definition of OMI BUT…
- 20 of these cases had acute culprit lesions (meaning they had an acute culprit lesion with TIMI 3 flow but a peak troponin lower than the set cutoff)
- Frequency and Findings of OMI ECG Patients:
- Hyperacute T-Waves: 49%
- Pathologic Q-Waves (Meaning Q waves associated with subtle STE which cannot be attributed to old MI): 47%
- Terminal QRS Distortion (Terminal QRS does not extend down to the baseline, with absence of both a J-wave and an S-wave): 53%
- Reciprocal STD and/or T-Wave Inversion: 82%
- Subtle STE not Meeting Criteria: 83%
- STD Maximal in V2 – V4 Indicative of Posterior OMI: 45%
- Any STE in Inferior Leads with any STD/T-Wave Inversion in aVL: 50%
- ONLY 6 CASES (4%) had none of these 7 findings, while 134 (92%) had ≥2 of these findings (Remember OMI criteria not solely based on ECG criteria alone…can use clinical picture, echocardiography, and troponin values)
-
The inclusion of cases was very difficult to assess. I had to read through this section a few times and still not sure I completely understand:
- Authors state: “Due to the rarity of OMI among all ED patients with Potential ACS, we had insufficient resources to perform a prospective, consecutive cohort study, and instead we performed a retrospective cohort study to maximize both the number of OMI patients and the number of Non-AMI patients with abnormal ECGs.”
- I believe they used cath lab records to identify patients initially
- This creates a huge selection bias as this is not all comers (Small denominator)
- Trial was done retrospectively in select patients. What would have made more sense is for the trial to have been done prospectively with all patients who received heart catheterization for suspected ACS (confirmation bias)
- To increase the number of cases the authors pulled in another cohort that had previously been collected for another study which was prospectively collected
- As there were not enough control patients with abnormal ECGs, a third database was referred to in order to add additional cases
- All of this to say…it’s complicated and it’s not the way these patients are identified in clinical practice
Author Conclusion: “Blinded interpretation using predefined OMI ECG findings was superior to STEMI criteria for the ECG diagnosis of Occlusion MI. These data support further investigation into the OMI vs. NOMI paradigm and suggest that STEMI(-) OMI patients could be identified rapidly and noninvasively for emergent reperfusion using more accurate ECG interpretation.”
Clinical Take Home Point: Despite the confusing recruitment methodology, this is another trial that shows that there is a subgroup of NSTEMI patients (i.e. STEMI (-) OMI), who have acute large vessel coronary occlusions with similar outcome severity to STEMI (+) OMI patients. Despite the similar outcome severity, STEMI (-) OMI patients are much less likely to receive emergent cardiac catheterization in an expedited fashion compared to STEMI (+) OMI patients. STEMI (-) OMI patients are an under identified subgroup of STEMI patients that would benefit from emergent cardiac catheterization.
References:
- Meyers HP et al. Accuracy of OMI ECG Findings Versus STEMI Criteria for Diagnosis of Acute Coronary Occlusion Myocardial Infarction. IJC Heart & Vasculature 2021. [Link is HERE]
- Khan AR et al. Impact of Total Occlusion of Culprit Artery in Acute Non-ST Elevation Myocardial Infarction: A Systematic Review and Meta-Analysis. Eur Heart J 2017. PMID: 29020244
For More Thoughts on This Topic Checkout:
- REBEL EM: The DIFOCCULT Trial – Time to Change from STEMI/NSTEMI to OMI/NOMI?
- REBEL EM: OMI-NOMI – Time for a Paradigm Shift
Post Peer Reviewed By: Anand Swaminathan, MD (Twitter: @EMSwami)
The post Upping Our ECG Game: OMI vs STEMI appeared first on REBEL EM - Emergency Medicine Blog.
