
 Background Information: Therapeutic hypothermia is the use of targeted temperature management to reduce neurologic sequelae resulting from the severe ischemia-reperfusion injury that occurs during cardiac arrest primarily from shockable rhythms.1 Although a mainstay treatment in the Advanced Cardiac Life Support (ACLS) guidelines, its use has been widely debated as beneficial in improving neurologic outcomes in post-cardiac arrest patients with non-shockable rhythms.2-7 Recent studies have also questioned the exact temperature at which patients should be cooled.8 The authors of this study sought to assess whether moderate therapeutic hypothermia, compared with targeted normothermia would improve neurologic outcomes in post-cardiac arrest patients who had a non-shockable rhythm.
Background Information: Therapeutic hypothermia is the use of targeted temperature management to reduce neurologic sequelae resulting from the severe ischemia-reperfusion injury that occurs during cardiac arrest primarily from shockable rhythms.1 Although a mainstay treatment in the Advanced Cardiac Life Support (ACLS) guidelines, its use has been widely debated as beneficial in improving neurologic outcomes in post-cardiac arrest patients with non-shockable rhythms.2-7 Recent studies have also questioned the exact temperature at which patients should be cooled.8 The authors of this study sought to assess whether moderate therapeutic hypothermia, compared with targeted normothermia would improve neurologic outcomes in post-cardiac arrest patients who had a non-shockable rhythm.
Clinical Question:
- Does moderate therapeutic hypothermia at 33oC or normothermia at 37oC improve the neurologic outcome in patients who have been successfully resuscitated out of cardiac arrest with a non-shockable rhythm?
What They Did:
- A multi-center, open-label, blinded-outcome-assessor, randomized control trial in 11 university hospital ICUs and 14 community hospital ICUs in France.
- Patients were randomly assigned using a 1:1 ratio to one of the following two groups:
-
- Moderate Therapeutic Hypothermia: With a targeted temperature of 33oC during the first 24 hours with a window of +/- 0.5oC. Slow rewarming was then performed at a rate of 0.25-0.5oC/hr to 36.5-37.5oC which was maintained over the next 24 hours
- Normothermia: With a targeted temperature of 36.5-37.5oC for 48 hours
- The trial protocol involved standardization of several variables including sedation, neuromuscular blockade and the management of expected adverse effects
- Sedation dosing adjustments were made to achieve a Richmond Agitation-Sedation Score of -5 in the hypothermia group and 0 in the normothermia group.
Cooling Methods:
- Active internal cooling using a specific device
- Active external cooling using a specific device
- Active external cooling without a specific device
Inclusion Criteria:
- Patients 18 years and older who suffered an out-of-hospital or in-hospital cardiac arrest with a non-shockable rhythm due to any cause.
- GCS ≤ 8 at ICU admission. If sedated before ICU admission, the last GCS determined by the ED physician just before sedation was used
Exclusion Criteria:
- No initiation of CPR or down time of more than 10 minutes
- Greater than 60 minutes of CPR (despite obtaining ROSC)
- Hemodynamic instability (ie. continuous epinephrine or norepinephrine infusion)
- Time from cardiac arrest to screening of more than 300 minutes
- Severe hepatic dysfunction as evident by Child-Pugh Class C Cirrhosis
- Pregnancy or breast-feeding
- Status of being under guardianship or being an inmate at a correctional facility
- Inclusion in another cardiac arrest RCT with neurologic outcome at 90 days as the primary endpoint
- Lack of health insurance
- Next of kin deciding for the patient to not participate
Outcomes:
Primary
- Survival with a favorable 90-day neurologic outcome assessed using a Cerebral Performance Category (CPC) score of 2 or less (Figure 1)
Secondary
- Mortality
- Mechanical ventilation duration
- ICU length of stay
- Hospital length of stay
- Infections
- Hematological adverse events
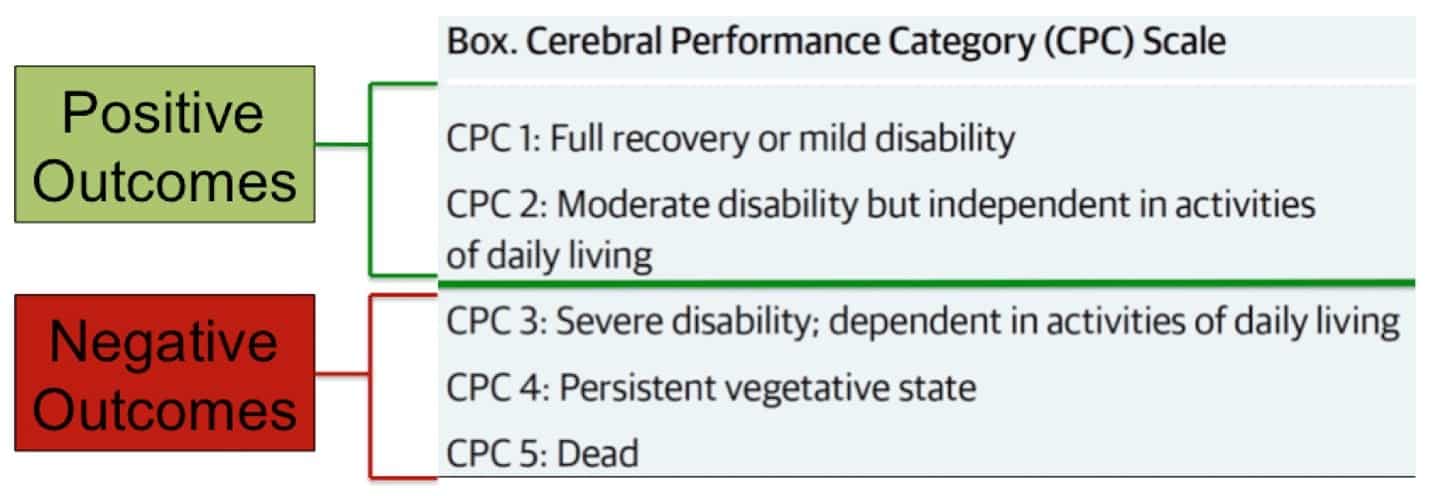
Figure 1: Breakdown of the Cerebral Performance Category Scale
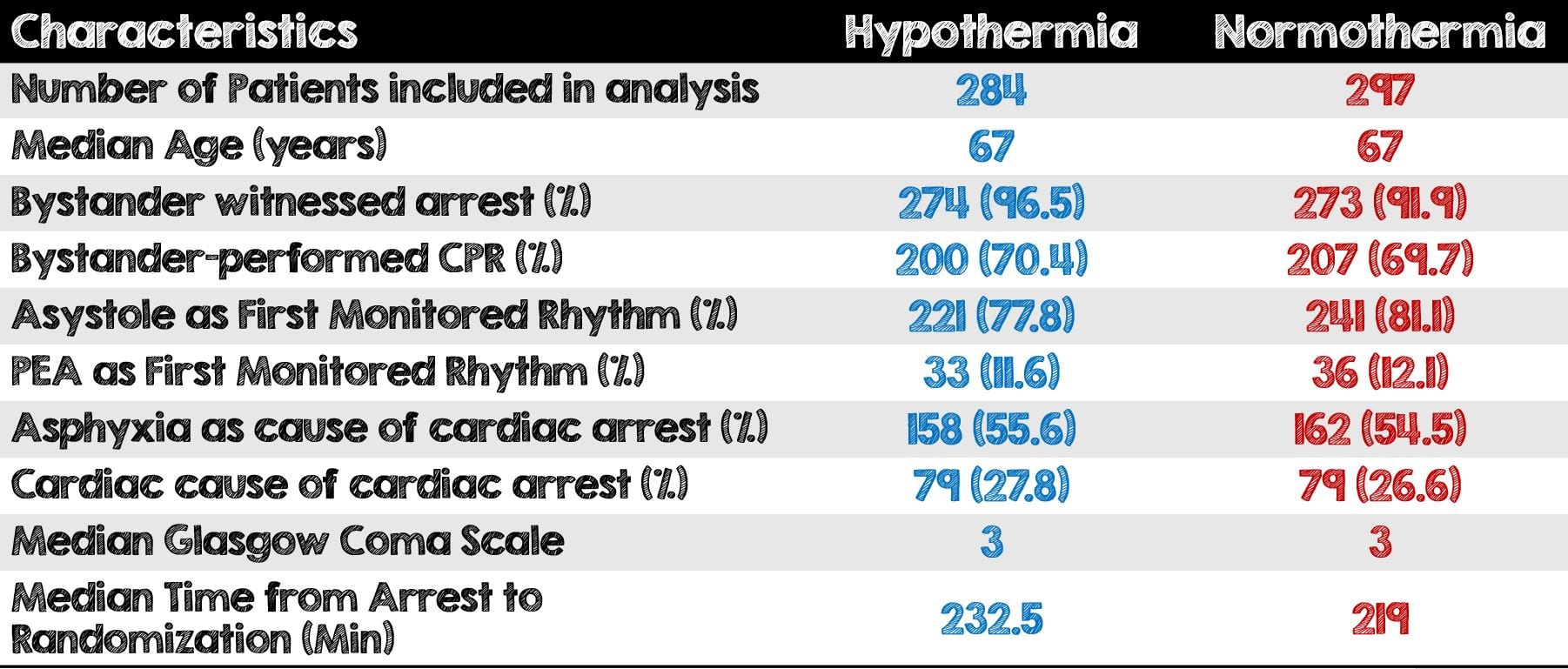
Table 1: Results and Characteristics between Hypothermia and Normothermia Groups
Results:
- Of the 2723 patients assess for eligibility, 506 (18.6%) had no CPR for greater than 10 minutes and 627 (22.9%) were excluded due to being moribund.
- In hospital cardiac arrest made up 27.4% of all the cases while Out-of-hospital cardiac arrest was 72.6% of cases
- The cause of cardiac arrest was non-cardiac in two-thirds of patients
- In the Hypothermia group, cooling began at a median of 16 minutes after randomization and stopped prematurely in 36 (12.7%) patients
Critical Results:
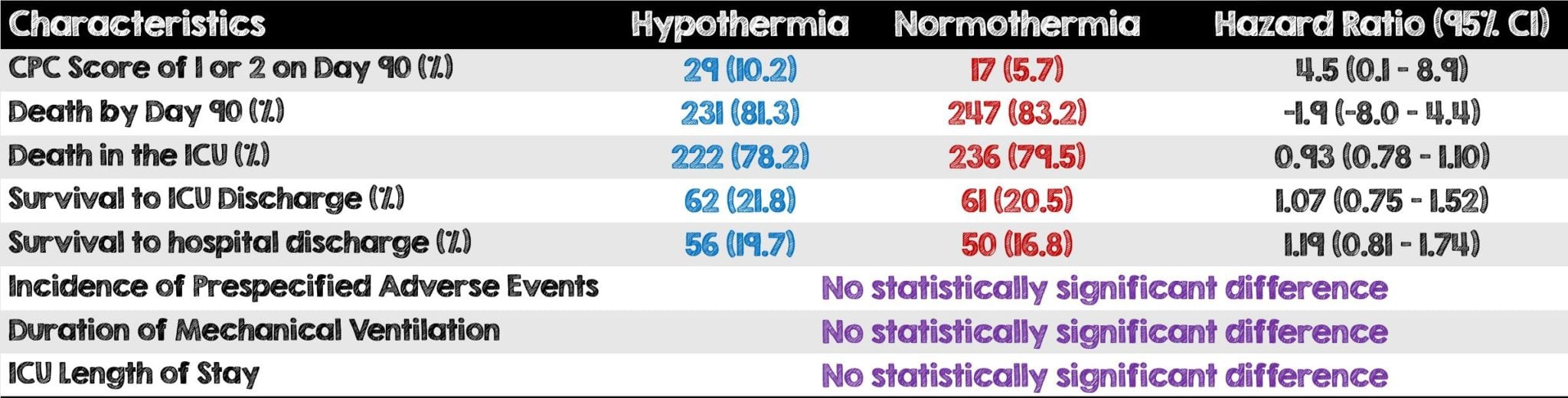
Table 2: Additional results and hazard ratio comparison between hypothermia and normothermia groups
Strengths:
- First study to look at the role of TTM in non-shockable rhythms
- None of the trial funders had any role in the trial design, collection or analysis of the data or the writing of the manuscript. Furthermore, the authors used both internal and external cooling devices, with no promotion towards one device or method over the other.
- Randomization of patients occurred using a web-based system that was available 24-hours per day. The randomization sequence was generated by a statistician, who was not involved in the recruitment of patients and performed stratification based on presumed cause of cardiac arrest
- In terms of baseline characteristics, patients were equally balanced between the two groups.
- Mix of community and university ICU settings adds to the study’s overall external validity or ability to be replicated
- Very pragmatic and “real” study replicating what the majority of hospitals do for their hypothermia protocols.
- Hyperthermia (above 37.5oC) was managed similarly in the two groups
- The authors used a widely understood (and validated) means of measuring neurologic function (ie. CPC Score)
- Wide variety of secondary outcomes relating to patient care, use of ICU resources and overall hospital costs
- In order to minimize confounding variables, there was a standardization of several parameters including sedation, neuromuscular blockade and management of expected adverse events
- Bleeding risk and ventilator associated pneumonia was the same in both groups. This finding was consistent with the previous targeted temperature management studies.8
Limitations:
- All study hospitals were located in one country thus limiting this study’s external validity and overall reproducibility.
- The investigators grouped together in-hospital and out-of-hospital cardiac arrest despite both having different causes and being treated differently.
- Study authors assumed that 23% of patients in hypothermia group and 14% in the normothermia group would have CPC scores of 2 or less on day 90 when in fact the numbers were much lower than this (10.2% and 5.7%).
- No flow and low flow times are very difficult to determine accurately. It is possible that patients who should have been excluded were actually included and vice versa.
- Substantial portion of patients in the normothermia group had fevers which could bias the results to favor the hypothermia arm
- Patients in the hypothermia group were more sedated than the normothermia group as evident by their RASS of -5 vs 0 in the normothermia group.
- Primary outcome was assessed during a phone interview rather than a face-to-face encounter. This may not be a truly accurate means of assessing how neurologically intact study subjects were. Furthermore, the telephone interview was done by only one psychologist blinded to the group assignments. The results may have been very different if the interview was done in real-time or with multiple psychologists.
- Targeted temperature management was used for a longer period (ie. 56 – 64 hours) in the Hypothermia group than in the normothermia (ie. 48 hours) which may skew the overall final results towards the TTM group.
- Patients with missing data were assumed to have died, this assumption was made to three patients. One in the hypothermia group and two in the normothermia group
- Use of fragility index value of 1 may have too heavily weighed the outcome as a single patient would make a difference in the primary outcome insignificant.
Discussion:
- In this trial, moderate therapeutic hypothermia improved neurologic prognosis but not survival at 90 days. It is difficult to ascertain whether the benefit in neurologic outcome was truly due to the intervention of hypothermia or the strict temperature control to avoid fevers. (Figure 2)
- The statistically significant benefit seen in the hypothermia group is very marginal. The phone interview having only been done by one psychologist may have been the reason the findings were significant. Had there been multiple psychologists or an additional means of validating the answers to the phone-interview the results could have been very different, and possible not statistically significant.
- The TTM study created lots of controversy regarding the exact temperature when their findings concluded that temperatures of 33oC were no better for neurologic outcomes than 36oC.8 While this study used 37oC for their normothermia, it provides no information as to which exact temperature for hypothermia is better for neurologic outcomes.
- It is important to note that this was a very sick population of patients as evidenced by the fact that 82.3% of the 581 patients died during follow-up. Furthermore, 58% of the patients in this study had circulatory shock compared to the 15% in the TTM trial.
- More patients in the hypothermia group had dedicated loop surface devices compared to the normothermia group which had a higher number of patients receiving basic external cooling (Table 3).
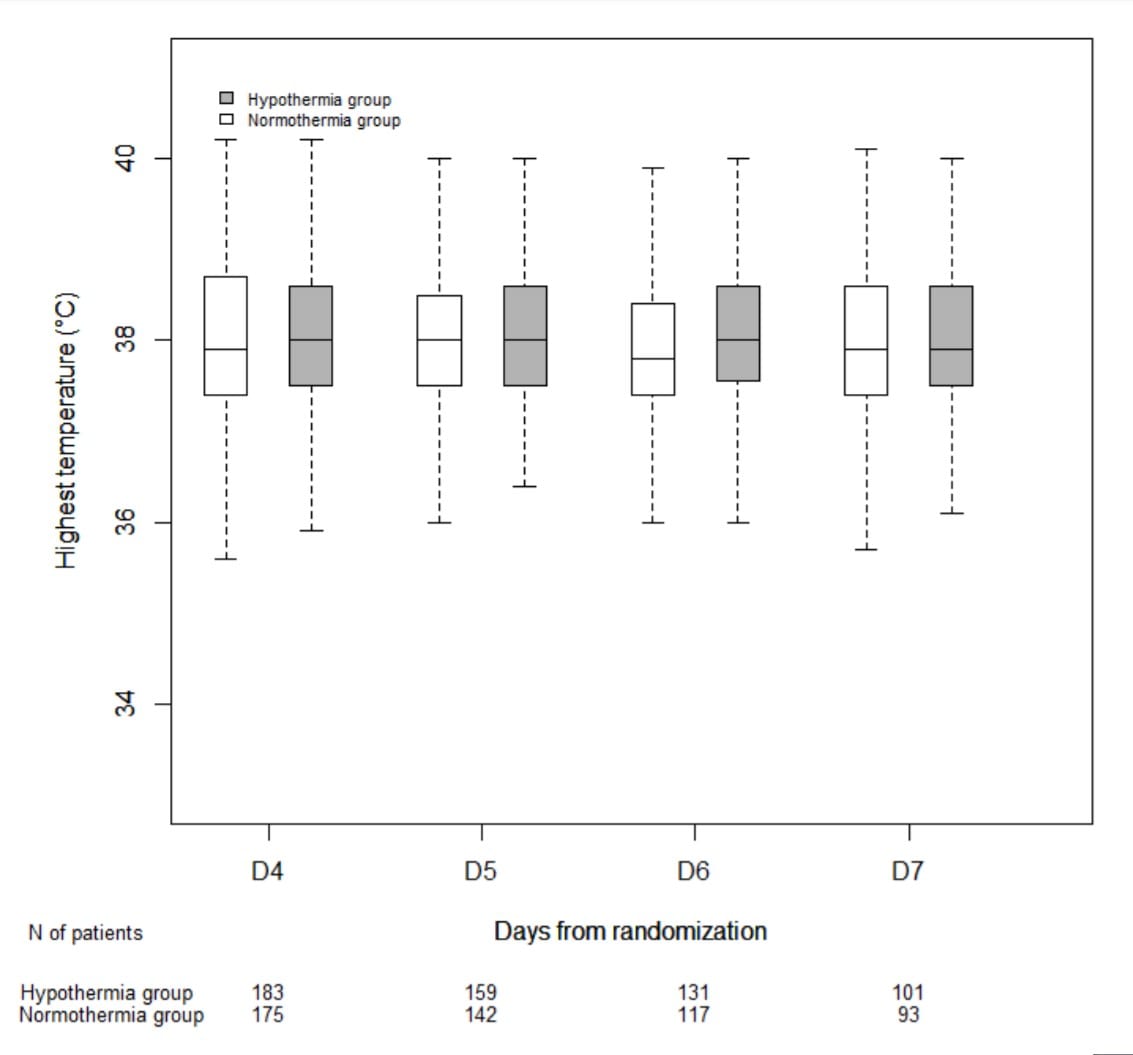
Figure 2: Changes in temperature between days 4 and 7 after discontinuation of physical cooling
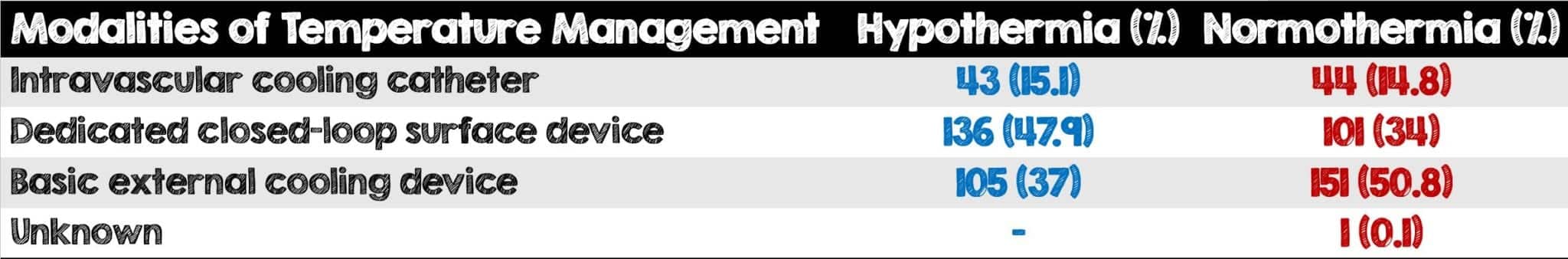
Table 3: Modalities of Temperature Management Used Among Both Groups
Author’s Conclusions:
- Among patients with coma who had been resuscitated from cardiac arrest with non-shockable rhythm, moderate therapeutic hypothermia at 33°C for 24 hours led to a higher percentage of patients who survived with a favorable neurologic outcome at day 90 than was observed with targeted normothermia.
Our Conclusion:
- This study emphasizes the importance of using definitive temperature control using an adaptive-control device. However, it provides no information about whether 33oC vs 36oC is preferable. Lastly, additional studies are needed to investigate more of the body’s effect at a temperature of 33oC and whether this or the avoidance of fever leads to better neurologic outcomes.
Clinical Bottom Line
- Therapeutic hypothermia may be neurologically beneficial for post-cardiac arrest patients with non-shockable rhythms however efforts should be directed at avoiding fevers in these patients.
Expert Opinion:
Benjamin S. Abella, MD, MPhil
Director, Center of Resuscitation Science
Vice Chair for Research, Emergency Medicine, University of Pennsylvania
Founder of Targeted Temperature Management Academy (Twitter: @PennTTM)
Twitter: @BenjaminAbella
- Is the neurologic benefit of TTM due to hypothermia or avoidance of fever?
It’s likely from BOTH lowering of temperature and from fever avoidance. We know that fever is very bad for the injured brain, so avoiding fever is important. But the laboratory data are quite convincing that there is a dose-effect to the benefit of temperature reduction (deeper post-arrest cooling in pig and dog models of arrest results in much better outcomes than higher temp set points)
- More patients in the hypothermia group had dedicated loop surface devices compared to the normothermia group which had a higher number of patients receiving basic external cooling. Based on your expertise what is the best cooling method we should be using and why?
The data are increasingly clear that precise temp management is better than sloppy temp management – so I’m a big supporter of “closed loop” cooling devices that are thermostatically controlled as opposed to simpler “cooling blanket” approaches without thermostatic regulation.
- One of the interesting aspects of this study was that patients in the hypothermia group were sedated to a RASS of -5 while patients in the normothermia group were sedated to a RASS of 0. Do you find this to be a major limitation of this study?
I don’t think it’s a major limitation, but agree that it’s a confounder – the data on sedation and paralytic use post-arrest with regards to outcome is unclear, so it’s hard to know how big a deal this is
- Targeted temperature management was used for a longer period of time (ie 56 – 64hrs) in the hypothermia group and only 48hrs in the normothermia group. Do you think this skews the overall final results towards the TTM group?
Another confounder; might have although it seems the amount of post-TTM fever was the same in both groups
- Following the findings of this study and your expertise in TTM, In what ways should community ED physicians change their practice if at all?
I think this RCT, coupled with a number of previous non-RCT studies that found statistical benefit to temp management to 33C for PEA and asystole arrest patients, suggests that community ED physicians should use TTM for most post-arrest patients who arrive in the ED, regardless of initial rhythms.
For More on This Topic Checkout:
- The Bottom Line: HYPERION
- PulmCrit: Hypothermia for Non-Shockable Arrest – Let’s Not Get Hot-Headed About This
- The SGEM: SGEM #275 – 10th Avenue Freeze Out – Therapeutic Hypothermia After Non-Shockable Cardiac Arrest
- First10EM: Hypothermia for Cardiac Arrest
REFERENCES:
- Lascarrou J-B, et al. Targeted Temperature Management for Cardiac Arrest with Nonshockable Rhythm. N Engl J Med. October 2019. PMID: 31577396
- Testori C, et al. Mild therapeutic hypothermia is associated with favourable outcome in patients after cardiac arrest with non-shockable rhythms. Resuscitation 2011. PMID: 21705132
- Perman SM, et al. The utility of therapeutic hypothermia for postcardiac arrest syndrome patients with an initial nonshockable rhythm. Circulation 2015; PMID: 26572795
- Vaahersalo J, et al. Therapeutic hypothermia after outof-hospital cardiac arrest in Finnish intensive care units: the FINNRESUSCI study. Intensive Care Med 2013; PMID: 23417209
- Dumas F, et al. Is hypothermia after cardiac arrest effective in both shockable and nonshockable patients? Insights from a large registry. Circulation 2011. PMID: 21321156
- Chan PS, et al. Association between therapeutic hypothermia and survival after inhospital cardiac arrest. JAMA 2016; PMID: 27701659
- Mader TJ, et al. Comparative effectiveness of therapeutic hypothermia after out-of-hospital cardiac arrest: insight from a large data registry. Ther Hypothermia Temp Manag 2014; PMID: 24660100
- Nielsen N, et al. Targeted temperature management at 33°C versus 36°C after cardiac arrest. N Engl J Med 2013; PMID: 24237006
Post Peer Reviewed By: Salim R. Rezaie, MD (Twitter: @srrezaie)
The post HYPERION: Targeted Temperature Management in Cardiac Arrest Patients with Non-Shockable Rhythms appeared first on REBEL EM - Emergency Medicine Blog.
