

Background Information:
Physicians have and continue to heavily contribute to the current opioid epidemic in the United States and Canada.1 Although much of the focus has been opioid prescriptions given to patients in the emergency department,2,3 not much attention has been paid to critically ill patients who survive to hospital discharge. The long-term sequelae of these opioids is concerningly overlooked especially when physicians utilize these medications as part of an “analgesia first” approach to sedating critically ill patients for the purposes of invasive mechanical ventilation (IMV).4 Previous observational studies in Canada found that approximately 85% of critically ill patients receiving IMV were exposed to opioids.1 Furthermore, the average daily opioid dosing for 2-7 days was 63 milligrams of morphine equivalent (MME), increasing to 106 MME per day for patients receiving IMV for greater than 7 days. The authors of this study performed a retrospective chart review of population-based data from Ontario Canada to investigate the frequency of new opioid initiation and persistent opioid use among critically ill patients who received mechanical ventilation. They compared this to patients who were hospitalized but not critically ill.
Clinical Question:
- What is the frequency of new and persistent opioid use among critically ill patients who received invasive mechanical ventilation?
What They Did:
- Retrospective review of Ontario healthcare databases including the Narcotics Monitoring System and the Registered Persons Database.
- Longitudinal follow-up of individuals, with regard to survival status and healthcare utilization, admitted to an ICU between February 1st, 2013 and March 31st, 2015 who survived at least 7 days following hospital discharge
- Compared cohort of critically ill patients requiring mechanical ventilation to another group admitted to the hospital, but not an ICU, during the same period and also survived for at least 7 days after discharge
Inclusion Criteria:
- Adult patients between the ages of 18 and 105
- Had to receive invasive mechanical ventilation in an ICU during their hospital stay
- Opioid naive (ie. not having filled an opioid prescription 90 days prior to hospitalization)
Exclusion Criteria:
- Patients who
-
- filled an opioid prescription within 90 days prior to hospitalization
- had an opioid overdose as a reason for hospitalization in the one year prior to enrollment
- had opioid overdose as the reason for the index hospitalization
- were less than 18 years of age or greater than 105 years of age
- received cardiac surgery during index hospitalization (given short duration of mechanical ventilation)
- were admitted to an ICU in the year prior to the index hospitalization
Outcomes:
Primary
- Percentage of patients who met criteria for persistent opioid use (defined as having filled a prescription within 7 days of hospital discharge AND filled 10 or more prescriptions in total or more than 120 days total supply within the first year after hospitalization)
Secondary
- Percentage of patients who filled an opioid prescription within 7 days after hospital discharge
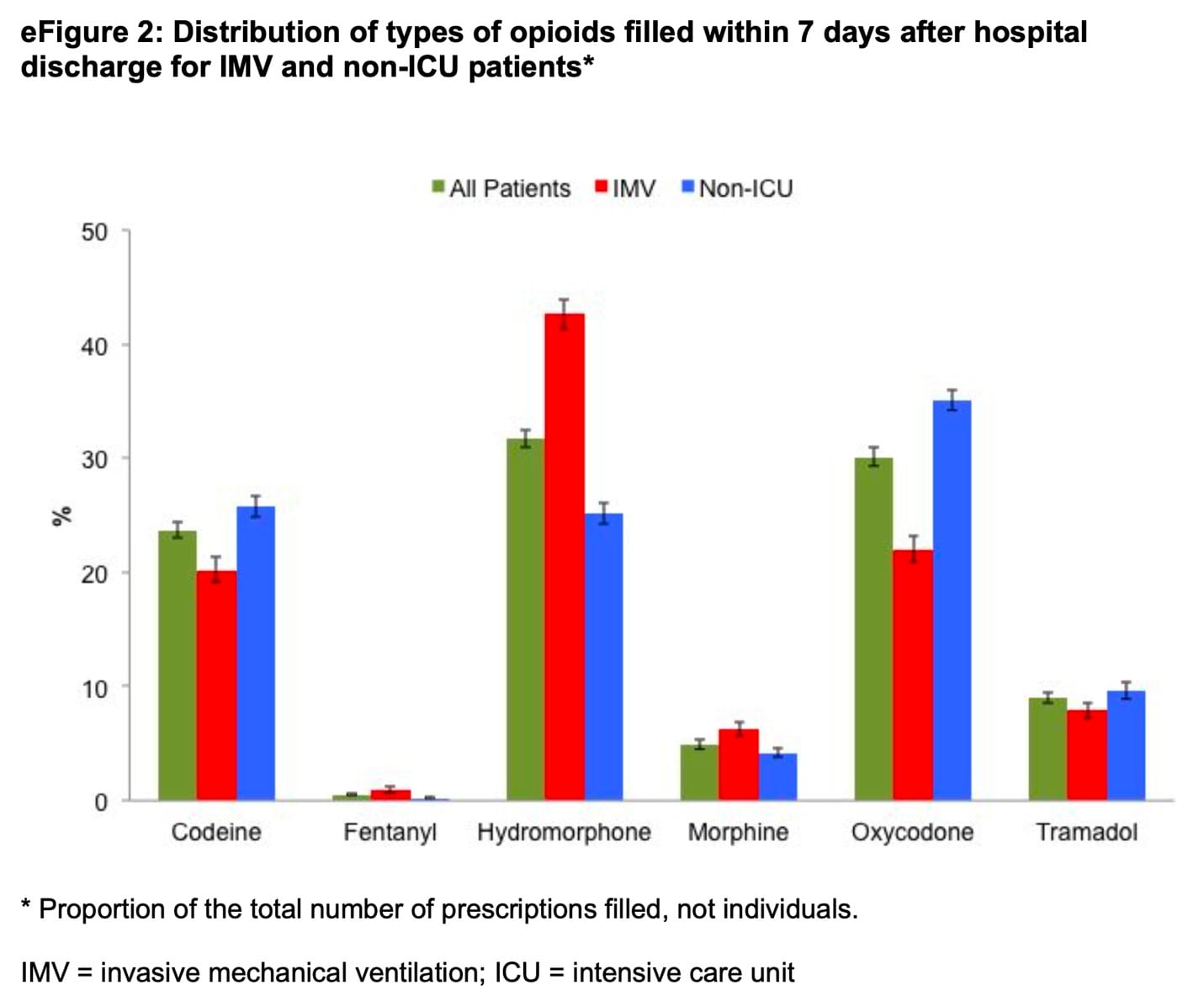
- Types of opioids dispensed in the first 7 days
- Daily and Total Dose (in milligrams of morphine equivalent) of opioid dispensed for initial filled prescription
Results:
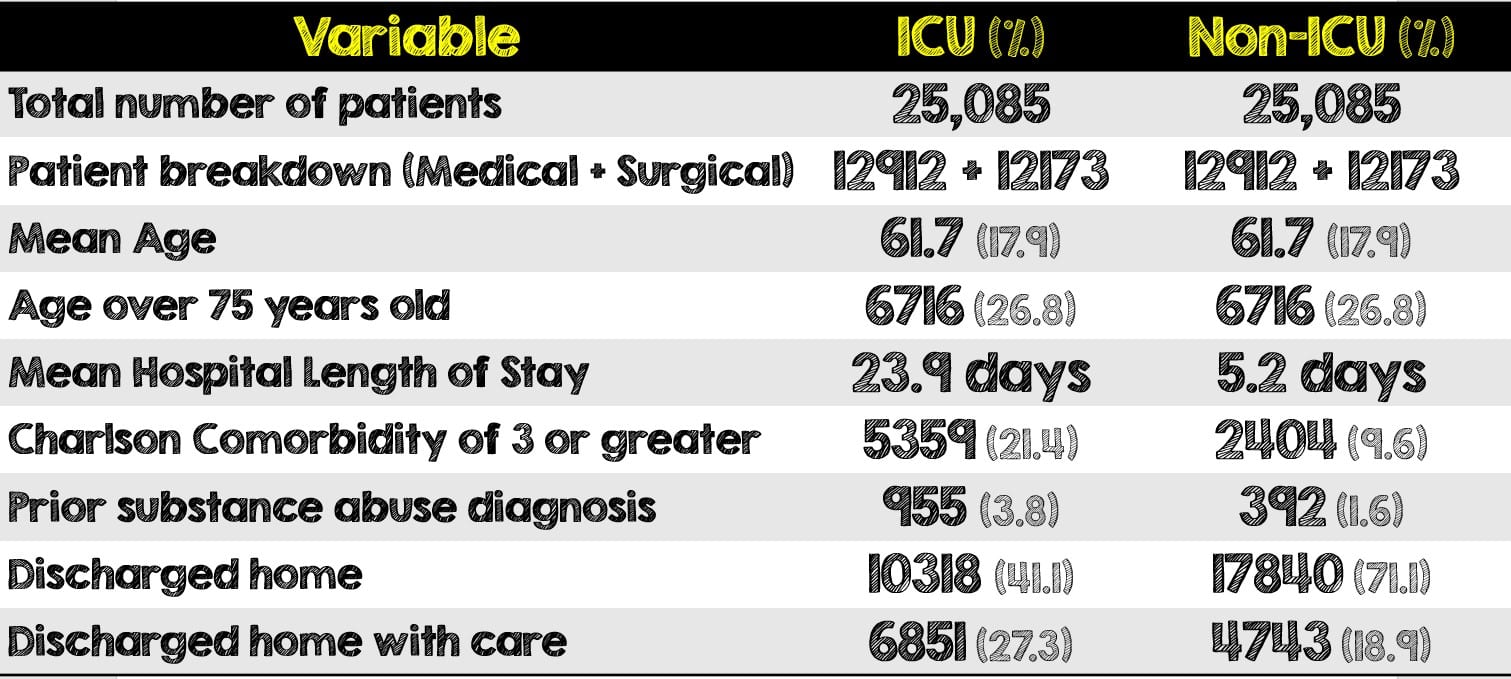
- 25,058 opioid naive patients were admitted to a hospital, received mechanical ventilation and survived at least 7 days following hospital discharge. They were matched to the same number of non-ICU patients
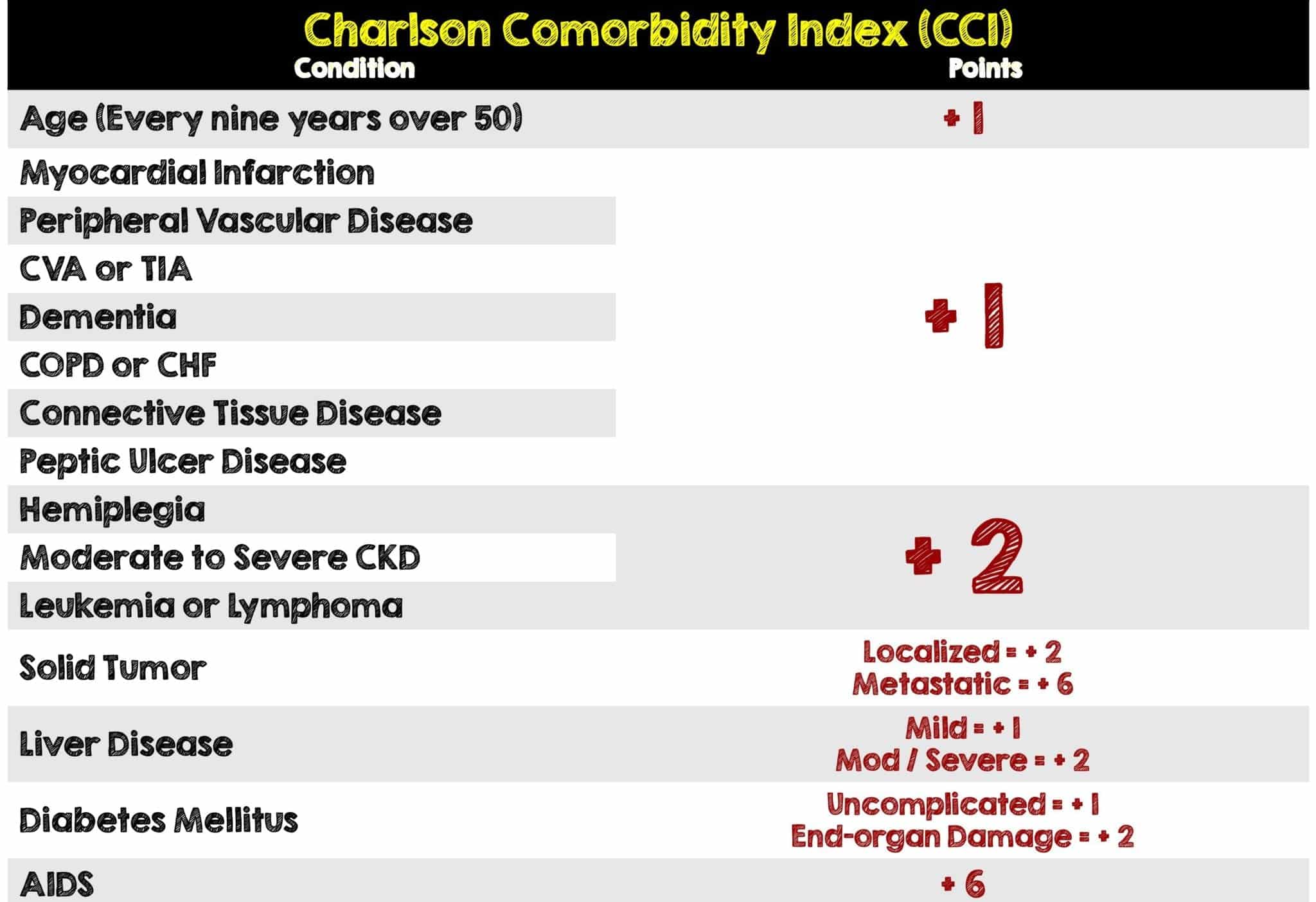
- More medical patients had three or more Charlson comorbidities (24.1% vs 18.5%, SD 0.14) and were more likely to have filled a benzodiazepine prescription in the year prior to hospitalization (21.7% vs 15.1%, SD 0.17). These patients had substantially shorter hospital length of stays (median of 11 vs 15 days, SD 0.33)
- During the hospitalization, the median duration of IMV was 3 days (IQR 2-6), with a median ICU length of stay of 6 days (IQR 3-11), and hospital length of stay of 13 days (IQR 7-27)
- 25.7% filled four or more prescriptions over the course of the year
- Hydromorphone was the most common initial opioid prescription (42.6%) followed by oxycodone and codeine.
- A greater percentage of surgical patients filled an opioid prescription within 7 days (33 vs 7.6% p<0.001)
Critical Results:
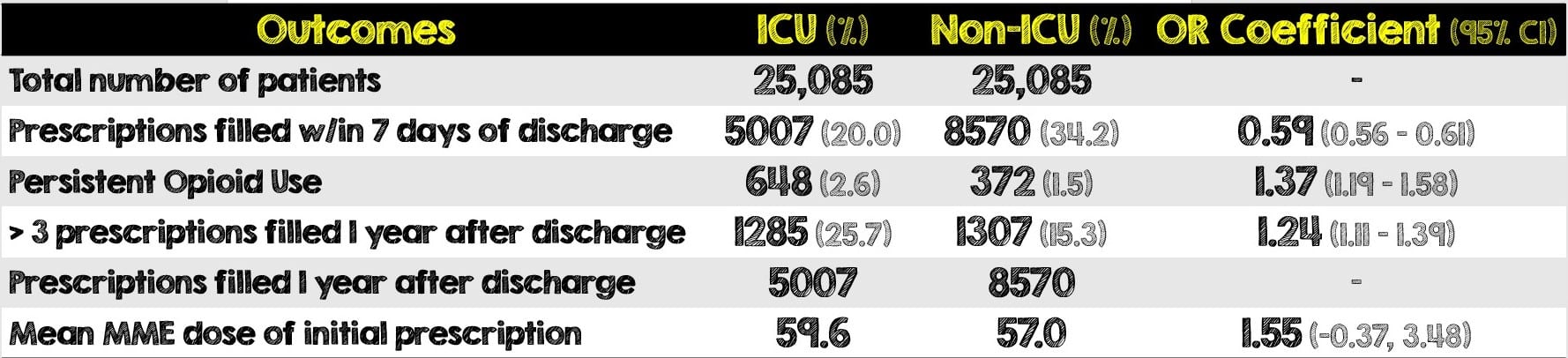
- Persistent opioid use was higher among surgical patients (4.0%) then medical patients (1.2%)
- The strongest predictor of filling an opioid prescription within 7 days of hospital discharge was being a surgical patient. Older patients (over the age of 75 years old) were also strongly associated.
- Individuals with more comorbidities and those who spent longer in the ICU were less likely to fill an opioid prescription following hospital discharge
Graph from [1]
Strengths:
- First study looking at the long-term impact of utilizing opioids on critically ill, mechanically ventilated ICU patients. Also had the ability to evaluate all adult patients admitted to ICUs over a large geographic region.
- Were able to capture all prescriptions filled (including those without insurance coverage) due to the requirement for all opioid prescriptions having to be recorded
- The authors had a very clear and well-defined criteria for persistent opioid use, thus allowing them to better search for these patients
- Due to variability in estimates associated with different definitions of persistent opioid use, the authors performed two post-hoc sensitivity analyses
- Utilized “greedy” matching. This is the pairing of cases in an ordered and sequentially matched method to the nearest unmatched control. If more than one unmatched control matches to a case, the control is then selected at random. Due to the large number of potential non-ICU patients available for comparison, all IMV patients were able to be matched.
- Assessed 14 baseline characteristics of patients such as Charlson comorbidities, prior diagnosis of mental illness or substance and even neighborhood median income quintile. These were then assessed again after the patients were stratified as medical or surgical admissions.
Limitations:
- Reproducibility is limited as this study cannot be replicated in a country that does not have a unified healthcare database or central tracking of opioid prescriptions such as Canada.
- Patient groups were considered unbalanced at baseline. The non-ICU patients had fewer Charlson comorbidities, less benzodiazepine use in the year prior to hospitalization and a greater proportion who were discharged directly home
- Unable to determine when the exact exposure of opioids occurred during hospitalization. Based on observational and trial data, the authors expect that at least 80% of the mechanically ventilated patients would have received IV opioids during their ICU stay
- In addition to timing being unknown, there is no mention of what opioid was given in-hospital, how much opioids and for how long during the patient’s hospitalization
- While opioid infusions are typically discontinued before transfer out of an ICU, the frequency of continued use in oral form on the wards is not well described in this study
- Could not determine the post-hospitalization pain of individuals or adjudicate the appropriateness of the opioid prescription.
- Did not assess patients for opioid use disorder and the authors recognize that persistent use is not the same as opioid use disorder
- Filling a single prescription may or may not mean the patient took the full amount or used any at all. These details are unclear from this study. However, filling multiple prescriptions has a high likelihood of actually taking the medication
- Although this study looked at income, history of substance abuse and history of mental illness, other important factors (ie. marriage, children, education, etc) that may have contributed to a patient’s risk of persistent opioid use were not assessed.
Discussion:
- The matching component of this study is an attempt to create an apples-to-apples comparison, however patients should have been matched to those who did not require mechanical ventilation instead.
- Patients in the ICU cohort, especially medical patients who spent more time there, had more Charlson comorbidities yet many of these variables were associated with lower odds of persistent opioid use.
- Patients in the ICU cohort were not discharged directly home and may have had a more complicated hospital and outpatient course requiring additional care/therapy when they left the hospital.
- Details of the in-hospital opioid course are underplayed. A patient on a short-course fentanyl drip immediately after intubation is very different from a patient requiring double-concentration Fentanyl for sedation and multiple doses of Dilaudid for their post-op pain
- Defined opioids as morphine, hydromorphone, fentanyl, codeine, oxycodone, meperidine or tramadol. Did not use Buprenorphine and methadone in their definition of new opioid exposure as these are primarily used to treat opioid use disorder
- Strength of the opioid matters. The more powerful the opioid, the greater the risk of taking too much and the more likely a patient will become physically addicted to the drug. At 7 days, hydromorphone was the most commonly prescribed opioid prescription followed by morphine and then codeine.
- The majority of patients (68.4%) were discharged home with or without home care and interestingly those who were discharged home with additional care were associated with increased odds of persistent use compared to those who had no care at home.
- On the other hand, the higher rates of persistent use observed in individuals sent to settings other than home provides an opportunity for intervention in these formal care settings
- The authors utilized the Narcotic Monitoring System which includes prescriptions for patients in skilled nursing facilities but not in acute rehabilitation facilities, specialized acute care facilities (ie. psychiatric) or chronic care facilities. For these patients, it is exactly unclear what was prescribed at these facilities. If it were in fact opioids it could contribute to their longer use.
- There are many factors that influence and contribute to persistent opioid use. Although not the focus of this study, the inclusion of these variables highlights an important reminder. Physicians should routinely be inquiring about the social support systems of all patients (both opioid-naive and opioid tolerant).
- For the emergency physician, this study should raise awareness on both the accurate assessment of all patients’ pain and the most appropriate medical therapy for their comfort. This is especially true for older patients with surgical emergencies, where mechanical ventilation and an ICU course may complicate their hospital stay.
Author’s Conclusions:
- Twenty percent of IMV patients received a prescription for opioids after hospital discharge, and 2.6% met criteria for persistent use, an average of 300 new persistent users per year in a population of 14 million. Receipt of surgery was the factor most strongly associated with persistent use
Our Conclusion:
- Mechanically ventilated patients, especially those who received surgery and required postoperative pain management, had increased risk of persistent opioid use when they filled a prescription within 7 days of hospital discharge to home. It is important to recognize persistent pain, particularly after surgical procedures, is a known concern and that not all persistent use of opioids represents inappropriate use. Furthermore, physicians should certainly not withhold pain medications from patients needing them, but rather assess the most appropriate treatment regimen for patients with many variables, including old age and multiple comorbidities, mentioned in this study.
Clinical Bottom Line:
- Physicians should use cautious clinical judgement and the most appropriate opioid therapy when managing patients’ pain, especially older patients who may require surgical intervention or mechanical ventilation. Providers should pay close attention to ensure medications started in the hospital are not required at hospital discharge. Frequent assessments of need should be undertaken in the hospital after a patient’s ICU stay, and in the outpatient setting to limit opioid use.
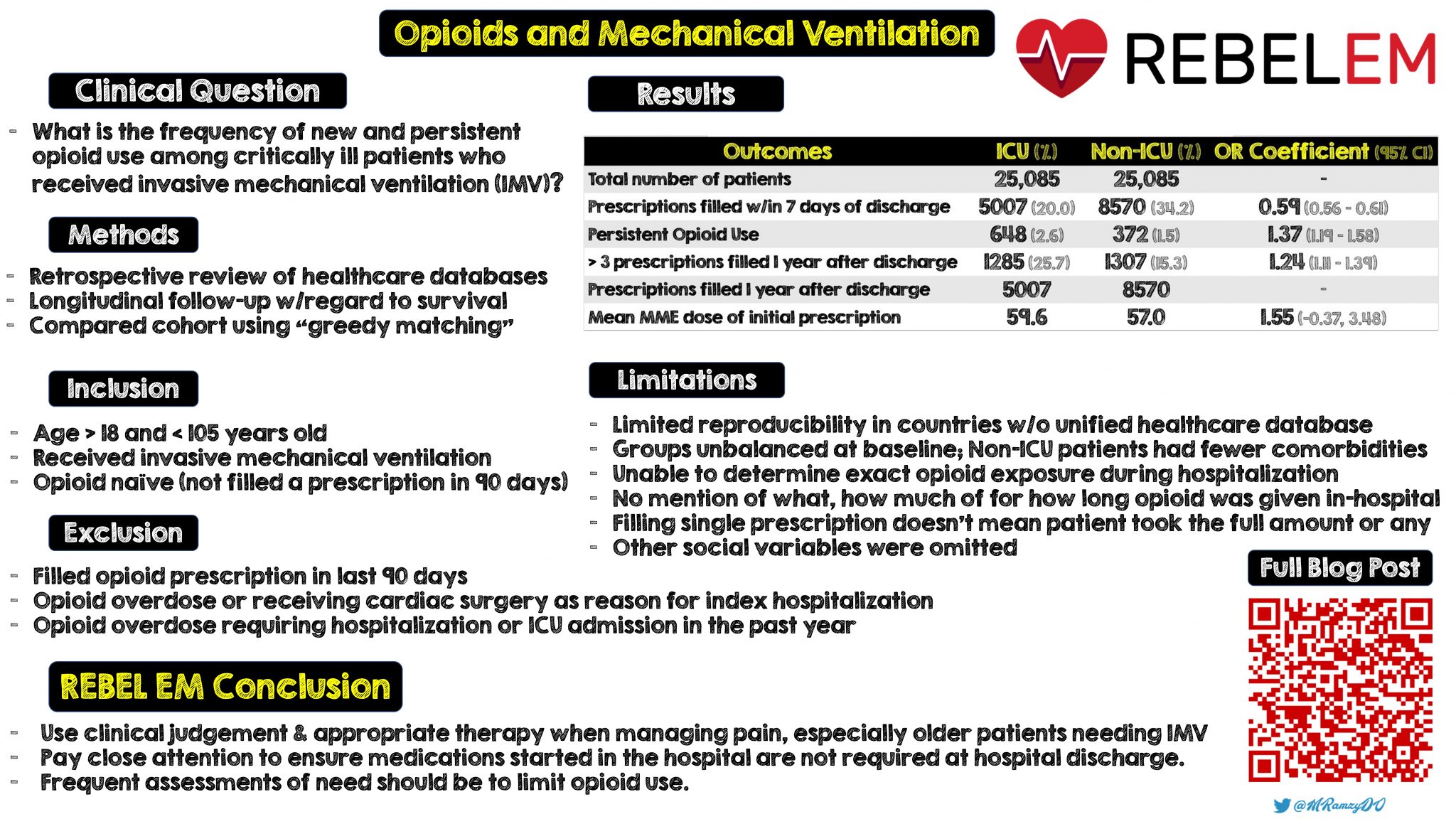 Summary Infographic Created by Mark Ramzy (Twitter: @MRamzyDO)
Summary Infographic Created by Mark Ramzy (Twitter: @MRamzyDO)
REFERENCES:
- Wunsch H, Hill et al. New Opioid Use After Invasive Mechanical Ventilation and Hospital Discharge [published online ahead of print, 2020 Apr 29]. Am J Respir Crit Care Med. 2020; PMID: 32348694
- Hoppe JA, et ak. Association of emergency department opioid initiation with recurrent opioid use. Ann Emerg Med. 2015; PMID: 25534654
- Barnett ML, et al. Opioid-Prescribing Patterns of Emergency Physicians and Risk of Long-Term Use. N Engl J Med. 2017. PMID: 28199807
- Barr J et al. Clinical practice guidelines for the management of pain, agitation, and delirium in adult patients in the intensive care unit. Crit Care Med. 2013; PMID: 23269131
Post Peer Reviewed By: Salim R. Rezaie, MD (Twitter: @srreziae)
The post New Opioid Use After Invasive Mechanical Ventilation and Hospital Discharge appeared first on REBEL EM - Emergency Medicine Blog.
