The MARCH Algorithm in Tactical Combat Casualty Care
by Andrew Fisher
this article was first published in September 2017 in The Havok Journal
Here is a link to the original article
The MARCH algorithm is synonymous with Tactical Combat Casualty Care (TCCC). It is a simple acronym for remembering the necessary steps in priority for saving lives in combat. M-massive hemorrhage, A-airway, R-respiratory, C-circulation, and H-hypothermia.
Recently EMS1.com published an article about the concept of the MARCH algorithm. While it is well known that civilian trauma and prehospital care advances greatly from military medicine during wars, at times, there is a failure of understanding about the meaning and reasoning behind the military’s rationale.
This article has a mix of concepts, assessments and treatments. It seems the author was applying MARCH to current trauma knowledge used in EMS. There are many areas where the article is spot on. However, there are a couple areas where information is incorrect or false. In other areas, it is vague and may leave the reader wondering why it’s done this way. Here is where the article could improve its message.
“MARCH is found in the tactical combat casualty care and advanced trauma life support courses.”
From what can be found, the MARCH acronym is most likely a UK invention. A thorough internet search failed to properly identify the origin. However, when a senior retired medical NCO, who is extremely familiar with TCCC was asked, he mentioned it was first heard around 2008 out of the UK military.
Advanced Trauma Life Support (ATLS) protocols were developed to standardize trauma resuscitation and provide a reliable method for the management of trauma patients. However, ATLS has never used the MARCH algorithm, this has always been a TCCC/military term. MARCH is used to identify and treat the major causes of preventable death. About 90% of all casualties in combat, die before reaching the hospital. We have an opportunity to save a small percentage of those casualties by using a methodical algorithm that allows for identification and immediate treatment of the life-threatening wounds.
MASSIVE HEMORRHAGE
“Massive hemorrhage can be addressed by the four Ds:
- Detect: find the source of the bleeding.
- Direct pressure: hold pressure on the source of the bleeding until the clot forms.
- Devices: if necessary, use equipment such as tourniquets, hemostatic gauze and pressure bandages to supplement direct pressure.
- Don’t dilute: use the concept of hypotensive resuscitation to avoid thinning the blood or pumping established clots.”
Massive hemorrhage is strictly about massive hemorrhage, the treatments include tourniquet application, which should be the first treatment applied in true massive hemorrhage. It is not unreasonable to apply a pressure bandage, if you do it should be a hemostatic dressing for compressible hemorrhage not amenable to limb tourniquet use or as an adjunct to tourniquet removal. Junctional tourniquets and the use of XSTAT® is also approved to control massive hemorrhage.
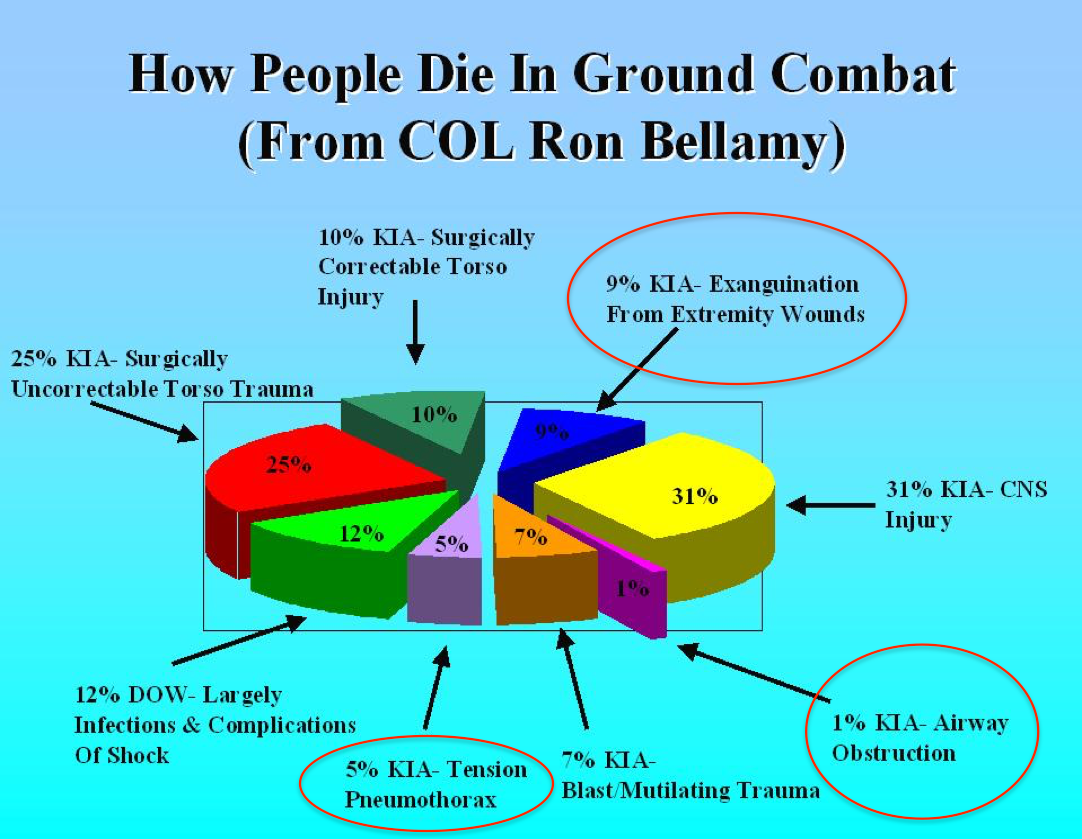
Hemorrhage is the leading cause of preventable death in combat. Bellamy (Figure 1) found that massive hemorrhage from extremities comprised over 9% of the all deaths in Vietnam. However, of the leading three causes of preventable death, it was about 60%. Similarly, Eastridge et al. (Figure 2) found 91% of the potentially survivable patients died from hemorrhage.
This is directly relatable to the civilian sector. Since 2001, there have been over 2,000,000 deaths from trauma. Over the last 10 years in the United States, there have been over 400,000 potentially survivable deaths, most of which were hemorrhage. Hesitation to immediately address massive hemorrhage is a significant reason to immediately apply a tourniquet.
The easiest, quickest, and most efficient method of hemorrhage control is by tourniquet application. If after addressing life threats, it is determined that the hemorrhage did not need a tourniquet, it can be converted. Two hours of tourniquet time is safe and they are used on a regular basis in orthopedic surgeries. Finally, there is no discussion of fluid resuscitation during the identification and treatment of massive hemorrhage.

AIRWAY CONTROL
“A reminds us that airway is still key care element for severe traumatic injuries. BLS to ALS, the patient needs a patent airway to survive.”
This tells me nothing about what to do with an airway, how to assess it or how to treat issues that arise. It does seem to imply it is appropriate to simply take a patient’s airway when the paramedic or EMT sees fit. Which also rolls into respiratory. If a patient can breathe on their own and maintain their own airway, they should. Studies demonstrate increased mortality with RSI and advanced airways.
In Bellamy’s study, airway occlusion only comprised 1% of the death, as opposed to Eastridge et al, where airway occlusion was 7.9%. What happened between Vietnam and the wars in Iraq and Afghanistan? It’s not clear, but it deserves more attention than the patient needs a patent airway. There are three types of patients that may present, the unconscious casualty that would require a simple jaw-thrust.
The conscious casualty with an airway obstruction or impending airway obstruction, may need basic airway maneuvers or insertion of an NPA. If these do not work, then a cricothyroidotomy (cric) is required. This is a major difference between the military and civilian medicine, but should be considered in EMS. The skill of intubation is difficult to teach and even more difficult to maintain. However, a cric is actually an easier skill, as it is a simple surgical procedure.
There is minimal training required and the maintenance training can be completed on manikins. Which technique should you use, according to a couple studies, the Cric-Key has been shown effective with fewer errors than the open technique. In civilian medicine, even the thought of a cric is frowned upon and may have some people asking questions.
There are various reasons for this, but in trauma, it may be a good option versus oral intubation (another EMS skill that has come under scrutiny in the last few years).
RESPIRATORY SUPPORT
“Assisting the patient with, or taking over respirations can move more air while simultaneously decreasing the patient’s respiratory effort using so much oxygen.”
Where is the assessment of the respiratory system to identify any thoracic trauma? The primary goal of the respiratory assessment is identifying penetrating chest trauma and a possible sucking chest wound. Once a chest seal has been applied, you should continue to monitor for a tension pneumothorax. Bellamy and Eastridge again, have differing numbers, 5% and 1.1%, respectively.
This could be for a variety of reasons, one possible explanation is the increased protection from body armor during the wars in Iraq and Afghanistan. Relating this to EMS, there might be a closer resemblance to Bellamy’s data and have a requirement for increased needle decompressions. In the military, the criteria for performing a needle decompression is low, the patient needs to have penetrating trauma and difficulty breathing.
This is due to the lack of certain types of medical equipment in combat. Typically, a stethoscope is not carried and one must rely on other methods to evaluate the pulmonary system. Other than the two mentioned criteria, altered mental status and weak or absent radial pulse are other signs. If a casualty has penetrating trauma, putting a 3.25 inch 14-gauge needle into his/her chest is not going to cause significant damage, it certainly will not cause a tension pneumothorax. Most importantly, if a tension pneumothorax is present, it will relieve it and save the patient’s life.
This is another skill that is frowned upon in EMS. There is utilization of chest seals in EMS, but rarely will a patient receive a needle decompression. In my eight years in EMS, I did exactly two. In fairness, it does take time for a tension pneumothorax to develop, and many inner-city services arrive at the trauma center before it can develop. Finally, there is no discussion on the use of end tidal CO2, pulse oximetry, the use of supplemental oxygen, all of which are used to monitor or treat a casualty.
He does get this right, but probably should have been mentioned sooner in his article.
“Keep in mind that over-ventilation can also do more harm than good. Ventilation provided with too much volume, speed or force can increase pressure in the chest, reducing blood return to the heart. This can have a negative effect on circulation, especially on trauma patients progressing towards shock.”
CIRCULATION
“The C in MARCH refers to shock. After massive hemorrhage, airway and breathing have been addressed, we need to optimize the patient’s circulation. Standard methods for circulation improvement, such as laying the patient flat, maintaining body temperature and careful fluid resuscitation all apply.”
This entire paragraph is wrong, shock assessment and treatment is addressed here, but it’s not the only thing. From an assessment point of view, one should identify other non-life-threatening bleeding, evaluate pulse and blood pressures. Like stethoscopes, in the combat setting, blood pressure cuffs are not used and guidelines recommend evaluating for shock with weak or absent radial pulse or altered mental status.
I believe, blood pressure cuffs should be carried and have carried one for the last several years. EMS is at a great advantage as there are blood pressure cuffs everywhere. Anything less than 80 mmHg systolic is considered hypotension and an indication of shock. For treatments, reassessment of any tourniquets applied, and if possible conversion should be completed, addressing the non-life-threatening bleeding, and starting a saline lock/gaining intravenous access.
This is where resuscitation begins, per TCCC guidelines in descending order of preference, whole blood, packed cells, plasma, and platelets 1:1:1, packed cells and plasma 1:1, either packed cells or plasma, finally Hextend and then Plasma-Lyte A. 0.9% sodium chloride or normal saline is not to be found anywhere in trauma resuscitation, and for good reason. Whole blood is sometimes hard to come by, but even here in the US, EMS units carry whole blood. As the author alluded too in the beginning, any resuscitation should be hypotensive resuscitation, no matter the fluid used.
He was also correct, in regard to diluting the intravascular volume, but that predominately occurs with Hextend and crystalloids (clear fluids). While most guidelines recommend resuscitating to a systolic of 90 mmHg, if using whole blood, it is probably safe to resuscitate to a systolic of 100 mmHg. Tranexamic acid (TXA) should be administered if you suspect the patient will get a blood transfusion. Finally, missing from this section is a discussion on pelvic binders to splint suspected pelvic fractures.
HYPOTHERMIA
He is absolutely right about this first sentence and cannot be emphasized enough.
“Hypothermia is a critical factor in trauma care that is not often discussed in the EMS.”
However…
“It is a key part of the so-called trauma triad of death, including hypothermia (low body temperature), H+ (acidosis, and which disrupts the blood’s ability to properly carry oxygen), and hypocoagulability (thinned blood or blood that has a reduced ability to clot).”
The issue with the lethal triad, it’s often iatrogenic…because a lot of folks in EMS still uses clear fluids to resuscitate trauma patients. It’s not the paramedics’ fault, they do not write the protocols. However, prehospital providers need to recognize the role they play in shock, and the author seems to allude to this issue.
Overall, the coagulopathy associated with hemorrhagic shock is probably more about the disruption of the coagulation cascade. Chances are, acute traumatic coagulopathy (ATC) is the bigger issue in trauma induced coagulopathy (TIC) (Figure 3). In TIC, both ATC and the lethal triad could be address with the use of whole blood and aggressive warming methods.

HEAD INJURY
“Head injury care is virtually all about making sure that a primary injury (the initial impact) does not turn into a permanent secondary injury (injury caused or worsened by inadequate EMS care). Care for patients with severe head injuries must avoid those H bombs:
- Hypoxia: even a momentary drop in oxygen saturation can cause permanent secondary brain injury.
- Hyperventilation: as already mentioned, too much or too fast ventilation can worsen shock. In addition, hyperventilation will blow off too much CO2, causing cerebral vasoconstriction, further decreasing perfusion to the brain.
- Hypotension: as intracranial pressure increases, the blood pressure required to perfuse the brain also increases. The rule of thumb is to avoid systolic blood pressure below 90 mm/Hg.
- Hypoglycemia: while there is nothing inherent to head injury that will drop blood sugar, an injured brain deprived of needed sugar will have a worse outcome.”
This discussion, is not necessary wrong and he provides a nice way to remember the issues associated with head injury. From the tactical field care perspective, head injury is not thoroughly addressed. There is more substantial discussion during the tactical evacuation portion of the guidelines, which to EMS, is more applicable. I’ll add, in the TCCC guidelines, “casualties with moderate/severe TBI should be monitored for:
- Decreases in level of consciousness
- Pupillary dilation
- SBP should be >90 mmHg
- O2 sat > 90
- Hypothermia
- PCO2 (If capnography is available, maintain between 35-40 mmHg)
- Penetrating head trauma.”
If there are signs and symptoms of cerebral herniation, the casualty should be treated with 250 mL, 3-5% hypertonic saline and hyperventilate the patient at a rate of 20 breaths per minute. The highest oxygen concentration possible should be used for hyperventilation. The casualty’s head should be elevated 30 degrees. Finally, there is nothing in MARCH about addressing hypoglycemia, but may be appropriate in EMS.
The MARCH algorithm can be expanded to include PAWS, which addresses P-pain medications, A-antibiotics, W-wounds, and S-splinting.
It is fantastic to see programs like TCCC and its associated methods (MARCH) making their way into civilian medicine and EMS. I know the author was well intentioned and wanted to share a great way to approach the trauma patient. It seems he was trying to take some standard EMS trauma care knowledge, apply the concept of MARCH, in order to improve on the current approach. I truly appreciate his efforts. However, there should be an understanding of why the point of injury care/battlefield medicine protocols are written in such a way and the evidence that supports it.
If you are looking to purchase some high quality M.A.R.C.H. tactical medicine products, you can visit the great selection of first aid and emergency medical products in our online store.





25 comments
Me gustaría aprender mas
Me gustaría aprender más sobre el curso para así tener más habilidad en situaciones de la vida real
La información del algoritmo MARCH me resulta sumamente valiosa, ya que proporciona una guía clara, priorizada y basada en evidencia para actuar ante situaciones de trauma en combate o emergencias ya que comprender la lógica de este protocolo me prepara para tomar decisiones rápidas y efectivas bajo presión, especialmente en escenarios de guerra o desastres, donde cada segundo cuenta. Además, me permite reforzar mi preparación como enfermero militar, al integrar conocimientos de medicina táctica, control de hemorragias, soporte respiratorio y prevención de hipotermia, lo que aumenta mis competencias clínicas y operativas para salvar vidas en entornos hostiles.
El artículo “The MARCH Algorithm in Tactical Combat Casualty Care” explica de forma clara y ordenada el protocolo MARCH, esencial en la atención táctica de heridos. Destaca por su lenguaje accesible y su enfoque en las causas de muerte prevenibles en combate, como la hemorragia y el compromiso respiratorio. La inclusión del modelo ampliado MARCH-PAWS demuestra una visión integral del cuidado prolongado.
Aunque es muy útil como introducción, se podría mejorar con ejemplos prácticos y referencias doctrinales oficiales. En general, es un recurso didáctico y efectivo para el personal militar y de salud táctica.
Considero que el algoritmo MARCH en la atención táctica de heridos en combate es importantes conocerla para todo el personal de sanidad, que aprendan a trabajar bajo presion, y puedan rescatar al personal que lo requiera, cada una de las fases es de suma importancia, recordarlas y realizarlas, desde el control de la hemorragia masiva hasta el control de la hipotermia, se agradece que se nos brinde esta informacion
El protocolo que seguimos es esencial para la primera atención que se le da a la persona en combate, march es el protocolo que mas se acerca a una buena valoración e inmediata para salvaguardar la vida de la persona asi mismo la atención a otros tipos de lesiones.
En las ejercicios militares de aplicación me enseñaron este protocolo personal de la escuela de sanidad pero aún que lo sigo escuchando he aprendido cosas nuevas acerca de él, su importancia en situaciones cotidianos donde ocurriera un accidente marca una gran diferencia el conocimiento de este protocolo y brindar el apoyo a personal civil.
El artículo de Andrew Fisher sobre el algoritmo MARCH ofrece una perspectiva valiosa sobre cómo los principios de atención táctica a heridos en combate pueden integrarse en la medicina civil, especialmente en entornos prehospitalarios. Sin embargo, su aplicación debe ser precisa y bien entendida. La crítica que se hace al artículo resalta una verdad importante: adaptar procedimientos militares a EMS requiere más que entusiasmo; requiere evidencia, contexto y claridad clínica. La prioridad de salvar vidas en el campo —controlando hemorragias masivas de inmediato y evaluando adecuadamente las vías respiratorias, respiración, circulación e hipotermia— debe guiar también la práctica civil, especialmente en traumas graves. Este tipo de debates y revisiones son esenciales para que la atención prehospitalaria evolucione basada en resultados y no solo en protocolos tradicionales.
El artículo me pareció muy interesante la información contenida permite que obtengamos los conocimientos para los profesionales de la salud que no sólo nuestra profesión ees en un hospital si no también intrahospitalaria
Es un acrónimo simple para recordar los pasos necesarios de manera prioritaria para salvar vidas en combate. M-hemorragia masiva, A-vía aérea, R-respiratoria, C-circulación e H-hipotermia
Me parece que el curso es de suma importancia para nosotros del área de la salud lo cual siento que es una gran oportunidad para nosotros dónde podremos adquirir conocimientos muy necesarios que nos pueden ayudar en cualquier momento necesario
Excelente información, muy concreta y resumida e interesante.
Me sirvió mucho para comer más a fondo del método MARCH para poder atender una urgencia médica en el campo de batalla
¡Excelente artículo! Me parece muy positivo que se difunda de manera tan clara y concisa un enfoque estructurado como el de las “cuatro D” para el manejo de la hemorragia masiva. Resaltar la importancia de la detección temprana, la presión directa como medida inicial crucial y la incorporación de dispositivos como torniquetes y vendajes hemostáticos es fundamental para mejorar la supervivencia. Además, enfatizar el concepto de reanimación hipotensiva para evitar la dilución de la sangre y la alteración de los coágulos es un punto clave y a menudo pasado por alto.
Es muy valioso que el autor conecte la experiencia del campo de batalla con el ámbito civil, mostrando la relevancia de estas estrategias para reducir las muertes evitables por hemorragia en ambos contextos. Las estadísticas presentadas sobre la alta mortalidad asociada a la hemorragia, tanto en entornos militares como civiles, subrayan la urgencia de una intervención rápida y eficaz.
La recomendación de priorizar la aplicación temprana de torniquetes en casos de hemorragia masiva y la aclaración sobre su seguridad durante las primeras dos horas son mensajes importantes y potencialmente salvavidas. La omisión intencional de la reanimación con líquidos en la fase inicial del manejo de la hemorragia masiva también es un punto crítico que merece atención.
En cuanto al control de las vías aéreas, es positivo que se destaque la necesidad de una vía aérea permeable para la supervivencia. Si bien el autor critica la falta de detalles sobre la evaluación y el tratamiento, el énfasis en no intervenir innecesariamente en pacientes con vías aéreas y respiración adecuadas es una consideración importante para evitar complicaciones. La mención de la cricotiroidotomía como una habilidad potencialmente más accesible que la intubación en ciertos contextos de emergencia también es un punto interesante para la reflexión en el ámbito del SEM.
Respecto al soporte respiratorio, la identificación de la evaluación del traumatismo torácico como un componente clave es acertada. La discusión sobre la posible mayor prevalencia de neumotórax a tensión en el ámbito civil, en comparación con los datos más recientes del campo de batalla, es una observación relevante para los profesionales de emergencias médicas. La cautela sobre la ventilación excesiva y su potencial efecto negativo en la circulación es un recordatorio importante.
En la sección de circulación, la crítica a la reanimación con líquidos claros y la recomendación de priorizar la sangre completa y otros hemoderivados en la reanimación del shock hemorrágico es una postura muy positiva y alineada con las guías actuales basadas en la evidencia. La mención del ácido tranexámico (TXA) y las fajas pélvicas como elementos importantes en el manejo del paciente traumatizado también es valiosa.
Finalmente, la inclusión de la hipotermia como un factor crítico en la tríada mortal y la conexión con el uso inadecuado de líquidos claros en la reanimación es una observación perspicaz. La mención de la coagulopatía traumática aguda (ATC) como un problema importante en la coagulopatía inducida por trauma (TIC) añade profundidad a la discusión.
En relación con la lesión craneal, la nemotecnia de las “bombas H” (hipoxia, hiperventilación, hipotensión, hipoglucemia) proporciona una herramienta útil para recordar los factores que pueden empeorar una lesión cerebral secundaria. La inclusión de las recomendaciones del TCCC para el monitoreo y tratamiento de pacientes con traumatismo craneoencefálico moderado/grave, incluyendo el uso de solución salina hipertónica y la hiperventilación controlada en casos de herniación, es información valiosa. La sugerencia de considerar el manejo de la hipoglucemia en el ámbito del SEM también es pertinente.
En general, el artículo presenta información crucial de manera organizada y destaca la importancia de un enfoque proactivo y basado en la evidencia para el manejo del paciente traumatizado. La conexión entre la medicina de combate y la medicina civil es un punto fuerte, y las discusiones sobre las controversias y las áreas de mejora en el manejo prehospitalario son muy valiosas para fomentar la reflexión y la actualización de los protocolos. ¡Un aporte significativo para la comunidad de profesionales de emergencias!
Muy interesante la medicina táctica, se puede salvar muchas vidas para poder seguir sirviendo al país
Muy interesante la medicina táctica, se puede salvar muchas vidas para poder seguir sirviendo al país