The ADVANTAGE Hemorrhage Control Bundle
$90.00
$120.00
TQ-RAM Pressure Point Device
$29.00
SAM XT Extremity Tourniquet
$53.00
SWAT-T Tourniquet
$25.00
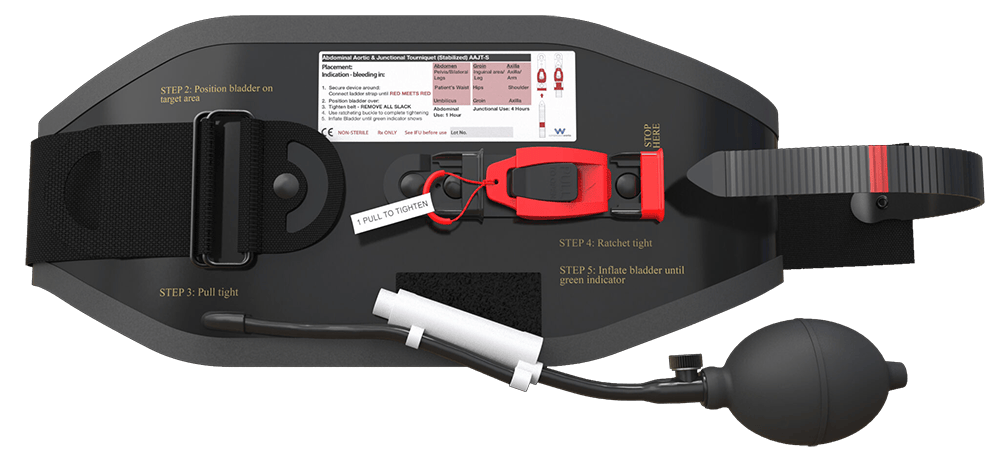
SAM® Junctional Tourniquet
$622.00
ITClamp Wound Pack Duo - Advanced
$141.00
$152.00
CELOX RAPID Hemostatic Wound Packing Gauze
$60.00
$71.00
Quickclot Combat Gauze Hemostatic Dressing
$63.00
$83.00
CELOX Rapid Ribbon
$47.00
The Advantage® Pressure Bar
$36.00
The HEMGUARD® Targeted Pressure Bandage
$13.00–$14.00
Slishman Pressure Wrap
$19.00
Slishman Pressure Wrap POUCH
$10.00
MARCH Battle Wrap
$21.00
TacMed™ Control Wraps
$4.00–$5.00
MARCH™ Battle Bandage
$25.00
$30.00
OLAES Modular Trauma Dressing
$11.00–$13.00
Israeli T3 Bandage
$17.00–$1,621.00